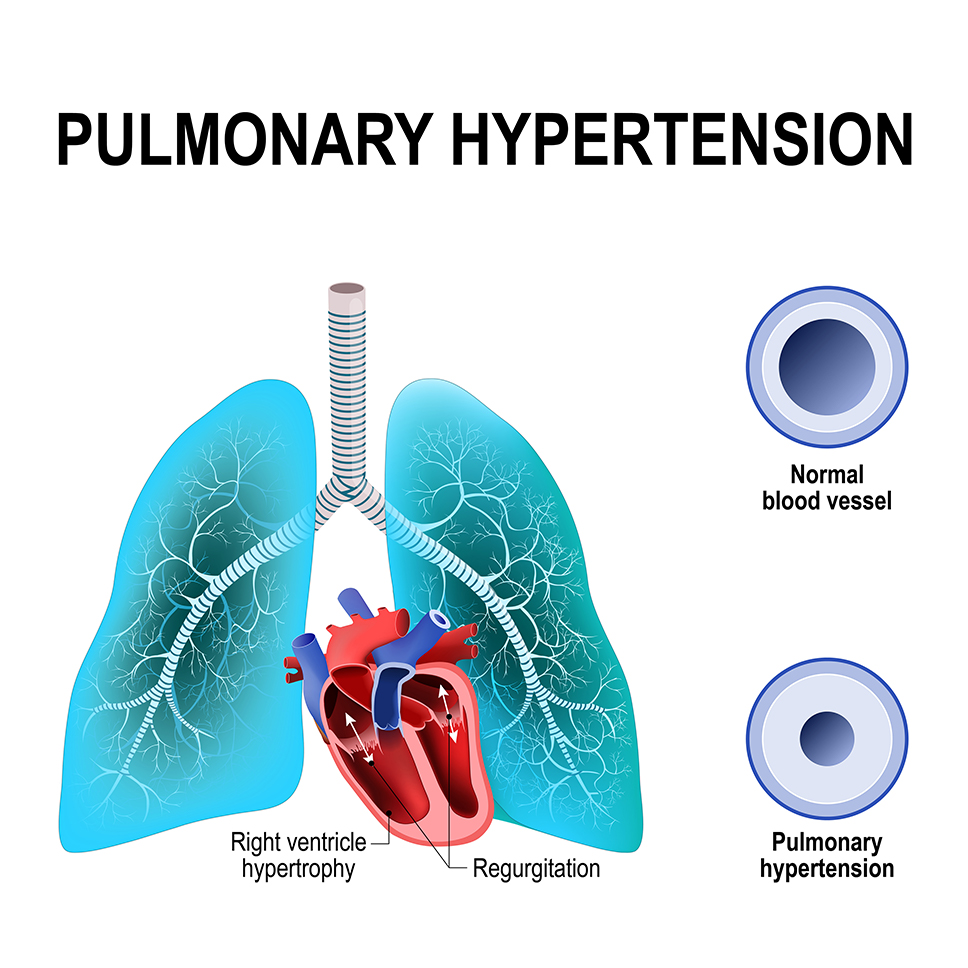
Chronic Thromboembolic Pulmonary Hypertension (CTEPH) is a rare form of pulmonary hypertension that occurs when blood clots, or thrombi, form in the arteries of the lungs and do not fully dissolve.
deep vein thrombosis | Dr Raghu
Pulmonary embolism is a blockage in one of the pulmonary arteries of the lungs. The most common reason for pulmonary embolism (PE) is a blood clot (thrombus) that travels to the lungs from other parts of the body (usually a leg).
When a blood clot (thrombus) is formed in one or more of the deep veins of your body (usually in the legs), it is known as deep vein thrombosis (DVT). Sometimes this clot becomes detached from the inner walls of the blood vessel and travels to another part inside the body. DVT may develop due to an underlying medical condition particularly the one which affects the clotting of the blood.

Causes and risk factors:
It can be caused by the factors which prevent the normal circulation of the blood and it’s clotting, such as long periods of rest (during a particular medical condition), injury to the vein, surgery and certain medications.
The risk factors are as follows:
- Inherited blood clotting disorder
- Prolonged bed rest
- Surgery
- Pregnancy
- Contraceptives or hormone replacement therapy
- Obesity
- Smoking
- Cancer
- Heart failure
- Inflammatory bowel disease
- Age (usually older than 60 years but can also occur at any age)
Complications:
The following are the complications which may arise due to DVT:
Pulmonary embolism: In Pulmonary embolism, a thrombus present in another part of your body usually a leg, travels to the blood vessel of the lung and blocks the blood circulation, leading to a life-threatening condition.
Post-phlebetic syndrome (post thrombotic syndrome): set of signs and symptoms seen after a blood clot has formed.
Symptoms:
The person may be asymptomatic during the formation of the thrombus, however, during post thrombotic period when it has caused damage to the veins, the blood flow to the affected body part may be compromised. The following symptoms are observed:
- Persistent swelling of the leg or arm (edema)
- Leg pain or tenderness while standing
- Skin discoloration in the affected arm or leg
- Veins in the arm or leg appearing larger than normal
Sometimes the development of a serious health complication such as pulmonary embolism is responsible for the symptoms in the DVT patients which are as follows:
- Shortness of breath
- Chest pain
- Cough (blood may be coughed out as well)
- Back pain
- Profuse sweating
- Lightheadedness
- Blue nails or lips
These symptoms appear suddenly, and an immediate medical attention is required.
Diagnosis:
The diagnosis is initiated by a thorough clinical examination and involves review of the patient’s medical history. Based upon these findings, the physician will categorize the patient into low or high risk DVT. Further tests may be considered to rule out other health problems and to confirm the diagnosis, which are as follows:
- Blood tests: These are considered to evaluate any blood disorders that increase risk of DVT.
- D- dimer test: In this test, the levels of a protein called D-dimer is assessed. In patients with DVT, high levels of this protein can be found in the blood.
- Duplex ultrasonography: It is a non-invasive evaluation of the blood flow in the arteries and the veins of a patient. But this test is not preferred for a thrombus located very deep inside the body such as pelvis.
- Venography: It is a specialized type of an x-ray procedure wherein a dye is injected into a vein of the foot, and the blood clot if present is detected.
- Magnetic resonance imaging (MRI): It is performed in patients for whom ultrasound examination is inappropriate or unfeasible. It can even detect a thrombus present in the patient’s pelvis and the thigh.
Prevention:
A recent World Thrombosis Day Ipsos survey showed that there is less awareness of DVT in countries around the world. Thus, the first step in prevention is making the public aware of DVT. The preventive measures are different depending on the person’s condition who are at risk of developing DVT:
During pregnancy
In pregnant women, certain medication may be prescribed if she has risk factors such as likelihood of having a cesarean birth, bed rest, history of DVT, and inherited thrombophilia.
During travel or in longer hours of sitting posture:
- Drink lots of fluids.
- Wear loose fitting clothes.
- Walk and stretch at regular intervals.
- Use special stockings to improve blood flow and to prevent blood clots but consult your health care provider before using it.
Treatment:
Treatment for DVT includes certain medicines and therapies, which are as follows:
Medications:
- Anticoagulants: They prevent further formation of blood clots but don’t dissolve the already existing ones. Most common anticoagulants used are heparin and warfarin. Warfarin is not recommended during pregnancy.
- Thrombin inhibitors: These are recommended for people who can’t take heparin.
- Thrombolytic medicines: These are recommended only during life threatening condition.
Compression stockings:
It may be recommended to prevent swelling and to avoid post-thrombotic symptoms in the patients.
Surgical treatment:
Surgical treatment may be performed when medications fail to dissolve the clots.
Thromboembolism refers to a condition where a blood clot formed in the blood vessel unplugs itself and flows in the blood stream to block another blood vessel leading to obstruction of blood flow. Although clotting is a normal bodily function, if a clot occurs where it is not required, it may lead to serious problems.

Types of Thromboembolism:
The type of thromboembolism differs depending on the area in which the clot may appear. It can obstruct the blood flow in the veins, arteries, brain, gastrointestinal tract or kidneys.
Thromboembolism can be further classified as below:
Venous Thromboembolism:
A venous thromboembolism is a thrombus (blood clot) formed in a vein. The blood flow in the veins is slow when compared to arteries which can increase the likelihood of the blood clots forming in these vessels.
It can be categorized into three different types
- Superficial Vein Thrombosis
The clot may occur in a superficial vein, close to the surface of the body. Usually, it is not serious until it enters the deep veins.
- Deep Vein Thrombosis (DVT)
Deep vein thrombosis occurs within the deep veins, and mostly occurs within the legs.
- Pulmonary embolism (PE)
Pulmonary embolism is a medical emergency in which the thrombus blocks the blood vessel in the lungs.
Renal Vein Thrombosis (RVT)
A renal vein thrombosis is a thrombosis that occurs in the veins that drain blood away from the kidneys. These clots reduce the ability of the kidneys to clean and filter the blood.
Arterial Thrombosis (atherothrombosis)
Arterial thrombosis is much less common than venous thrombosis. It can have similar risks. Usually arterial thrombosis may lead to necrosis of the tissue.
A thromboembolism in the coronary artery can cause a heart attack. If blood supply to the brain is disrupted, the patient may suffer a stroke.
Symptoms:
Signs and symptoms of venous thromboembolism include the following
DVT
- Pain in arm or leg, usually in the thigh or calf
- Swollen leg or arm
- Reddening or warming of the skin
- Red streaks on the skin
PE
- Shortness of breath
- Chest pain under your rib cage that can get worse when you take a deep breath
- Rapid heart rate
- Feeling lightheaded or passing out
- Accentuated second heart sound
Arterial Thrombosis
- Muscle pain or spasm in the affected area
- Numbness and tingling in the arm or leg
- Pale color of the arm or leg (pallor)
- Weakness of an arm or leg
If the condition is severe, it may lead to blister formation and shedding of the skin, leading to tissue necrosis.
Symptoms of a clot in an organ vary with the organ involved but may include:
- Pain in the part of the body that is involved
- Temporary decrease in organ function
Causes:
The blood clots can occur due to injury to a vein, consequence of a surgery, use of certain medications and lack of movement of the limbs.
In the case of PE, the blood clot may block the blood vessels of the lungs. The affected portion of the lung may die due to loss of blood supply, the condition is called as pulmonary infraction, making it difficult to provide oxygen to the rest of the body.
Occasionally, the blood vessels can be blocked by substances other than blood like collagen, part of a tumour, air bubbles etc.
Risk factors:
The common risk factors include
- Inheriting a blood-clotting disorder
- Prolonged immobility which may be due to bed rest or long trips
- Injury or surgery
- Pregnancy
- Birth control pills or hormone replacement therapy
- Being overweight or obese
- Smoking
- Cancer
- Heart failure
- Inflammatory bowel disease
- Family history of deep vein thrombosis or pulmonary embolism
Diagnosis:
The diagnosis of thromboembolism includes the following tests which could be considered depending on the type:
D-dimer: The blood sample is tested for the presence of D-dimer which is a marker for the presence of blood clots.
Duplex Ultrasound: This is an imaging test in which the presence of clots is identified using ultrasound waves.
Pulse oximetry: In this test, a sensor attached on the end of the finger of the patient helps to measure the level of oxygen in the blood.
Arterial blood gas: The blood drawn from the artery is checked for oxygen levels present in it.
Chest X-ray: This test may not be useful in finding the presence of clots, but can help to rule out a clot.
Other diagnostic tests may include ELISA, pulmonary angiography, venography, echocardiography, helical computed tomography of pulmonary vessels etc.
Treatment:
Treatment of thromboembolism includes:
Blood thinners: These are anticoagulant drugs which prevent formation of new clots while the body works to break up the previous clots present. They include heparin, low-molecular-weight heparin, apixaban, edoxaban, rivaroxaban, and warfarin.
Clot-busting drugs: These are intravenous injections to dissolve the clots in the case of life-threatening situations. They include drugs belonging to the class of tissue plasminogen activators.
Surgical and other procedures:
- Removal of clot: Surgery is considered only if the condition is life threatening. The clot is removed using a catheter threaded through the blood vessel.
- Vein filter: A catheter can also be used to position a filter in the inferior vena cava which helps to stop the clots from being carried into the lungs.
Prevention:
If the patient is at a risk of the condition, the following preventive measures may be considered to reduce the occurrence:
- Use of blood thinners
- Use of compression stockings
- Use of intermittent pneumatic compression devices that automatically squeeze the legs to keep blood flowing
Other preventive measures include
- Regular exercise
- Maintaining healthy weight
- Cessation of smoking
Consideration during travel include
- Walk every 1 to 2 hours
- Stretch legs and move around on the seat
- Drink lots of fluids
- Avoid smoking and consumption of alcohol before journey