“The advantages of cardiac xenotransplantation might result in the gradual replacement of heart allotransplantation by xenotransplantation (at least) in resource-rich countries” – Dr David Cooper
April 2022 Newsletter
-
Man gets a pig’s heart and survives for 2 months
-
Polygenic Risk Score – A novel modality for risk assessment in cardiovascular disease
-
Aortic Valve Replacement – TAVR versus SAVR – Which is durable?

Dear Readers,
Happy New Year day – Ugadi in Telugu and Kannada speaking areas, Gudi Padwa in Maharashtra and Konkan area, Puthandu in Tamilnadu. What can be a better time for us to re-start the Hearty Life newsletter.
This new avatar of Hearty Life is digital as the preferred medium keeping in trend with the changing reading habits of Gen X and Gen Z. In addition we have every issue online from now on. The previous issues’ archives would also be made available online soon.
The current issue of Hearty Life has interesting articles on a human being receiving a porcine heart transplant, a new risk score for predicting high risk coronary artery disease – Polygenic Risk score .
We have two digital cases that I encourage to share with your colleagues:
- TAVR in a patient with cardiac arrest and saving her
- Salvaging dialysis fistulas – which are precious for the vast number of patients
on dialysis.
This issue I am bringing from the Apuan Riveria of Tuscany, Italy. I am working at various cath labs in this region for nearly six weeks to upskill and keep abreast with the latest techniques in Interventional Cardiology. These sojourns stimulate me, brings the enthusiasm of childhood in me and gets me the foremost question in many peoples minds – What gives me happiness? During this sojourn I realised my happiness lies in learning and doing new, stimulating things and challenging my intellect as well as being in the company of highly skilled colleagues who are ever there to help and guide. I said to myself once again – “It is the company that matters”. Next issue I will share my Italian experiences and how the medical system is organized in Italy.
I hope this reincarnation of Hearty Life suits your interests and you find the articles as stimulating as I find myself writing them.
Love you all,

Enjoy reading !
Dr C Raghu
- MD (AIIMS); DM (NIMS); FACC; FESC; FSCAI
- Level 2 Master in Structural Heart Interventions
- Harvard writing scholar
- (www.asterprime.com)
- Hyderabad 500016, India
- Website: www.drraghu.com
- Twitter: @raghucardio | LinkedIn: Raghu C
Man gets a pig’s heart and survives for 2 months

Many of us read the story of a 57-year man who had end-stage heart failure; not fit for cardiac transplantation and thus received a pig heart. This is a genetically engineered pig’s heart which was grown in a controlled, bio-sealed environment. Post-surgery the pig heart was not rejected, survived 60 days and the cause of death would soon be known through a scientific publication.
Now let us look at the long and short of this story.
This ‘clinical experiment’ was based on work extending back 35 years and was made possible by advances in genetic
engineering of pigs, organ preservation technologies as well as in the development of novel immunosuppressive agents.
Polygenic Risk Score – A novel modality for risk assessment in cardiovascular disease
Case Report:
Mr. AM, a 28-year male has been admitted to the hospital with chest discomfort and sweating. The doctor has diagnosed him to have an acute heart attack. The family and friends of AM were aghast with this news
and surprised as he is a non-smoker, exercises regularly and has no diabetes and hypertension. Fortunately he recovers after an angioplasty and stent following which he recovers and gets back to work in the next 2 weeks.
This brings to fore the question – Why did Mr. AM have a heart attack at such a young age?
Traditionally, the risk for developing a heart attack is predicted by the presence of risk
factors – that are divided into modifiable and non-modifiable as shown in Table 1. Modifiable risk factors are those that can be controlled leading to reduction in heart events.
Table 1. Modifiable versus non modifiable risk factors for cardiovascular disease
| Non-modifiable risk factors | Modifiable Risk factors |
|---|---|
|
|
|
|
|
|
|
But many a time people who suffer a heart attack do not have these risk factors and still suffer heart attack. General public assumes that risk factors are needed for anyone to develop heart attack but research had shown that this is not necessarily true. Research had shown that only 30-40% of people who had heart attack had either diabetes, hypertension, smoking, high cholesterol, obesity etc. There are risk calculators such as the Framingham Risk Score, ASCVD plus risk score by the American College of Cardiology, Q risk score3, European Society of Cardiology risk score for the prediction of risk of development of heart disease in the next 5-10 years as well as
the life-time risk too. But these calculators predict the risk based on the traditional cardiovascular factors mentioned
in Table 1 which are present in only 30-40% of those who had myocardia infarction. Recently a novel genetic based risk score – Polygenic risk score – has been developed that can predict the risk of heart attacks using a different mechanism. Polygenic Risk Score (PRS) represents the aggregate contribution of the minor modifications that happen in the amino acid sequences in the human genome (alleles) l e a d i n g t o t h e d e v e l o p m e n t o f cardiovascular disease. Individually, the alleles’ contribution to the development of disease is mild to
In clinical medicine the utility of Polygenic Risk Score helps in risk prediction and screening algorithms for coronary artery disease, prioritization of patient subgroups that are likely to derive benefit from treatment, and efficient prospective clinical trial designs.
moderate but once aggregated into the PRS it has a powerful disease predictive ability.
How does PRS differ from previous genetic inheritance for cardiac disease?
One of the best studied genetic basis for heart disease has been Familial Hypercholesterolemia (FH) which is seen in 1 in 300 people leading to elevated LDL cholesterol and consequent severe atherosclerotic cardiovascular disease. In a study of young heart attack patients FH responsible genetic mutation was found in
3% of them documenting the fact that even though FH is a powerful causation for heart disease it is rare in occurrence. At the same time the FH gene mutation is a major change in gene pattern compared to the minor change seen with alleles that are accounted for in the PRS. PRS is an aggregation of the alleles whilst FH gene mutation is a single gene change leading to stronger inheritance pattern. Table 2 lists the differences between the traditional Mendelian inheritance of the diseases and the novel PRS system of disease prediction.
Table 2. Traditional Genetic risk factors versus Polygenic Risk score for Cardiovascular disease
| Non-modifiable risk factors | Modifiable Risk factors | Polygenic Risk Score |
|---|---|---|
| Modification of gene | Major – mutation | Minor – Allele |
| Disease association | Strong individual gene predictor | PRS is equally strong |
| Risk prediction for heart attack | 3-fold higher risk | 3-fold higher risk |
| Frequency | 3% of heart attack victims | 18% of heart attack victims |
| Therapeutic utility | Yes | Yes |
| Population level interventions | Not possible | Possible |
| Limitation | Uncommon mutation | Ancestry plays a major role in gene pool and PRS data for European population |
How do the traditional risk scores like Framingham Risk Score, ASCVD risk score fare against the PRS?
The traditional risk scores are Primary Prevention risk scores where as the PRS is a primordial risk score – we can estimate PRS even at birth also. This allows for the preventive strategies to be employed early
during life. Combining the traditional risk scores with the PRS enhances the risk predictive ability of either score alone.
At which PRS level confers a high risk of cardiac events?
The PRS level which is more than 95th percentile for that particular population
group confers a 3.4-fold higher risk.
What is the role of lifestyle modifications on an individual with high PRS?
People with high PRS when they participate in lifestyle modifications it has been found that the risk of cardiovascular events reduces to the level seen with low PRS levels.
Is the test available in India?
PRS have been tested in South Asians (India and Bangladesh) albeit to a much
lesser extent compared to European populations. It has been shown that PRS has similar predictive accuracy like that seen in the European populations especially in patients who presented with myocardial infarction less than 55 years.
This test is commercially available in our country through Medgenome.
Clinical Utility of Polygenic Risk Score:
1. High PRS may possibly used as “risk-enhancing factor” akin to what has been proposed in the 2019 ACC/AHA guidelines on Primary Prevention of Cardiovascular Disease.
2. High PRS level presents a strong window of opportunity to impress the individual on the need for life style modifications and early initiation of statin therapy.
3. C a r d i o v a s c u l a r t h e r a p e u t i c intervention clinical trials can be conducted only those groups of people with high PRS as a smaller number of patients may need be enrolled.
4. People with intermediate grade of coronary or cerbro-vascular disease and high PRS may be offered an early a n g i o p l a s t y – s t e n t t o r e d u c e t h e complications.
5. As a secondary prevention strategy people with high PRS and recent cardiovascular event need to be managed with aggressive risk factor reduction.
Conclusion:
Polygenic Risk Score is a novel parameter that helps clinicians identify people who are prone for high cardiac event rates. Over the last five years tremendous progress in Human Genome Project helped us to identify the gene alleles that could be responsible for precocious cardiac disease. The clinical utility of PRS in routine practice and its role in clinical role would be an interesting realm of clinical science.
Further Reading:
1. Klarin D, Natarajan P. Clinical utility of polygenic risk scores for coronary artery disease. https://doi.org/10.1038/ s41569-021-00638-w
2. Semsarian C, Ingles J, Ross SB, Dunwoodie SL Bagnall RD and Kovacic JC. Precision Medicine in Cardiovascular Disease: Genetics and Impact on Phenotypes: JACC Focus Seminar 1/5. JAm Coll Cardiol. 2021;77: 2517–2530
3. Tada H, Yeo KK, Li J-J et al. Polygenic Risk Scores for Atherosclerotic Cardiovascular Disease in the Asia-Pacific Region. JACC: Asia. 2021; 1: 294–302.
Aortic Valve Replacement – TAVR versus SAVR – Which is durable?
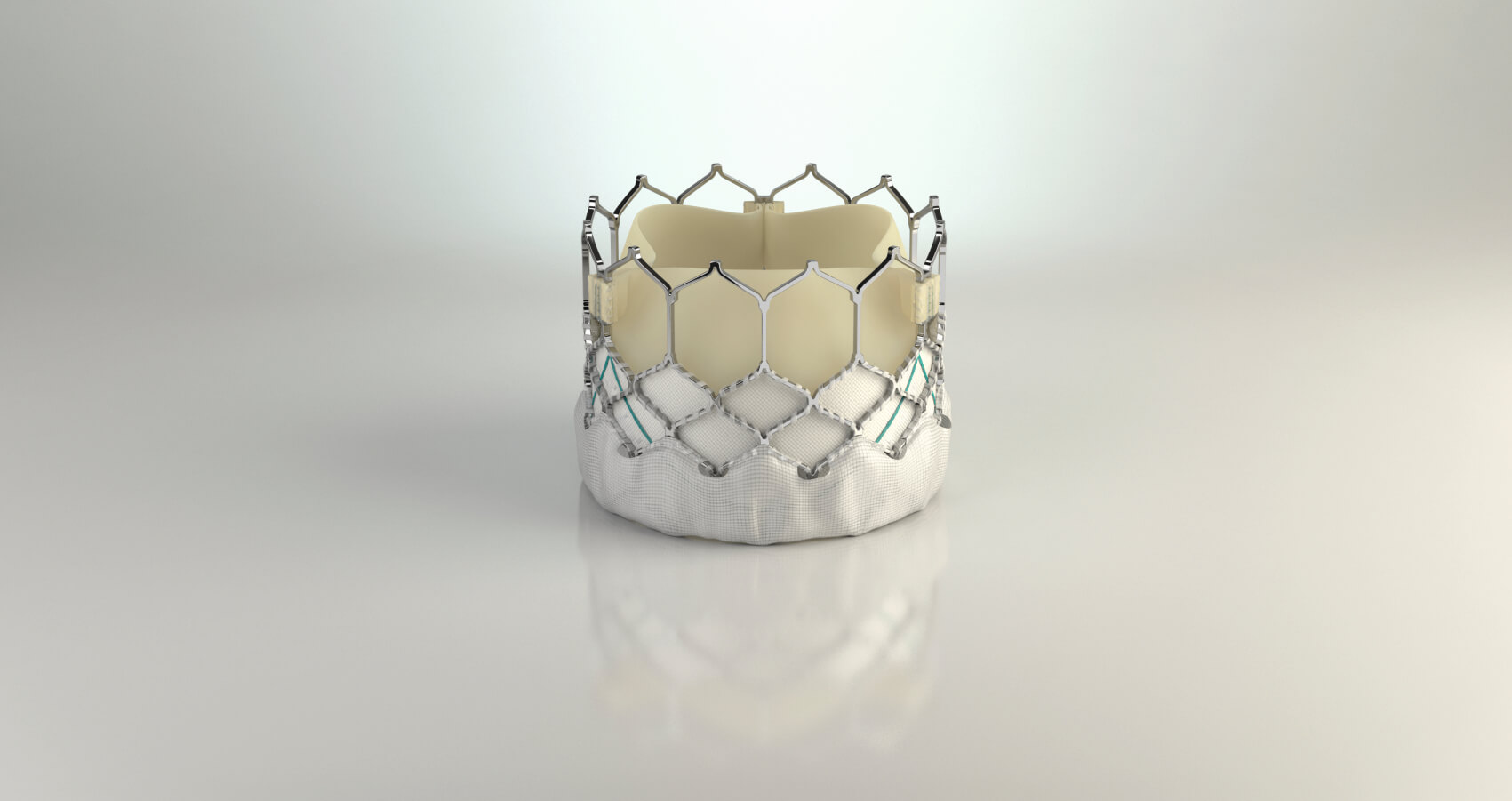
Transcatheter Aortic Valve Replacement (TAVR) is an elegant therapy for a challenging problem – Aortic Stenosis (AS). The time tested approach for managing AS has been Surgical Aortic Valve Replacement (SAVR). Unfortunately AS is a disease of the elderly and as many as 30-40% of patients are denied surgery because they are considered high risk for
SAVR. TAVR has emerged as a solution for this problem as it is less invasive, obviates the need for open heart surgery, can be performed even in the super old (>90 years), those with renal failure, previous history of cardiac surgery etc. Currently every year more than 200,000 TAVR are being performed globally.
SAVR is performed using two different types of heart valves – mechanical and bioprosthetic valve. Mechanical valves, made of metal alloys, are durable but would need the use of anticoagulant medicines life-long. Anti-coagulants prevent blood from clotting and are associated with heightened bleeding complications that cumulate over time. Bioprosthetic valves are made from processed animal tissue and closely mimic the native human valves. Unfortunately bioprosthetic valves also degenerate akin to human valves and the degeneration is in fact an accelerated one. Owing to this reason, bioprosthetic valves are recommended to be used for
more than 65 years of age. TAVR is the recommended choice of treatment for severe AS for more than 80 years of age across all risk categories. SAVR and TAVR are both suitable choices for the 65-80 years age group and the choice is determined through a shared decision making by the Heart Team. Choice of the valve is critically determined by the valve durability and the option for a simpler repeat replacement at a later date. This article will address the issue of which is durable – TAVR versus SAVR valve ? The main causes for a bioprosthetic valve dysfunction could include the following:
1. Valve degeneration due to calcification, fibrosis and tear of the valve.
2. Mismatch of the prosthetic valve to patient, suture leave away leading to paravalvular regurgitation.
3. Thrombosis
4. Endocarditis Data regarding the long term outcomes (>10 years) is still not available as these types of valves are relatively recent. SAVR valve is durable in 85% or more cases at the end of 10 years. The well established variable for early deterioration is young age at implantation.
In addition, renal impairment, smoking, arterial hypertension, dyslipidemia, diabetes mellitus, and metabolic syndrome are the other causes for accelerated degeneration of a bioprosthetic valve. TAVR therapy is a much younger therapy and in the initial phases it has been restricted to elderly high risk patients only. So the long term data is not available. A Dutch study with 7-year follow up showed 85% of patients are free from valve
degeneration. The PARTNER1 trial that compared head on TAVR versus SAVR at the end of 5 years had equivalent rates of valve degeneration. But in the CoreValve United States Pivotal High Risk trial at 5 years overall SVD was more common after SAVR than after TAVR (26.6% vs 9.5%). In the contemporary NOTION trial presented in 2020, comparing TAVR versus SAVR, bioprosthetic valve dysfunction is more after SAVR (24%) than TAVR (4.8%) at the end of 5 years.
Current data from registries as well as randomized controlled TAVR trials indicate that the medium- to long-term durability of THVs is satisfactory and at least non-inferior to surgical aortic bioprostheses.
This is of relevance as more younger and low ri s k patient s undergo TAVR. Cumulative data over the next few years involving younger patients will provide clear answer for this question.
E-case Report Corner
Through real world case scenarios we learn at the e-case report corner how modern medicine can be translated into daily practice. For everyone who follows these brief videos, can certainly learn tips in managing similar cases for future. It also provides an idea as to the gamut of interventions Dr. Raghu and team perform at their unit.
E-case Report April 2022
A 74 year female underwent TAVR procedure by Dr. Raghu and team. Severe aortic stenosis is a life-threatening disease and early valve replacement is essential. For patients who are not suitable for surgery TAVR is the best option for saving life. Sick patients with AS it is advisable for early TAVR rather than “wait and watch” policy. Let’s understand how this case is unique.
Click Here to view the video
E-case Report April 2022
Catheter-based therapy replaced surgical revision as the treatment of choice for failing or thrombosed dialysis fistulas and graft. Every effort should be made to salvage a failed dialysis fistula. It is criminal to loose a dialysis access site as they are precious. Through two cases we learn why dialysis fistulas fail and how “fistuloplasty” is the way to salvage failing fistulas.
Click Here to view the video

