A heart attack is a life-threatening condition that requires emergency medical interventions, such as angioplasty in the heart.
types of heart failure | Dr Raghu
There was a time when heart attacks were restricted to older people (in their 50s, 60s, or 70s). However, in today's day and age, heart attacks are becoming increasingly common in individuals under the...
Heart failure is a condition in which the heart can’t pump enough blood to meet the body’s needs. It’s a serious condition that requires treatment by your doctor, but there are several options available.
Congestive heart failure is characterized by a gradual deterioration in the heart’s ability to pump blood throughout the body. It can result in various symptoms, such as swelling in the abdomen, feet, and legs, shortness of breath, fatigue
Heart failure refers to a condition where the heart is unable to pump blood throughout the body with maximum efficiency. It’s usually the result of progressive weakening, thickening, or stiffening of the heart muscles.
Heart failure is a common condition with no known cure. However, proper treatment can control the disease progression and thus improve a patient’s quality of life and longevity. To decide the proper course of treatment, a doctor must first determine the type of heart failure a patient has developed.
Depending on the part of the heart’s pumping cycle that’s been affected, heart failure can be of two types – diastolic and systolic. You can learn more about the symptoms, causes, treatment of diastolic dysfunction and differentiation from systolic dysfunction in our previous article.
In this blog, we’ll delve deeper into systolic heart failure and understand its causes and symptoms.
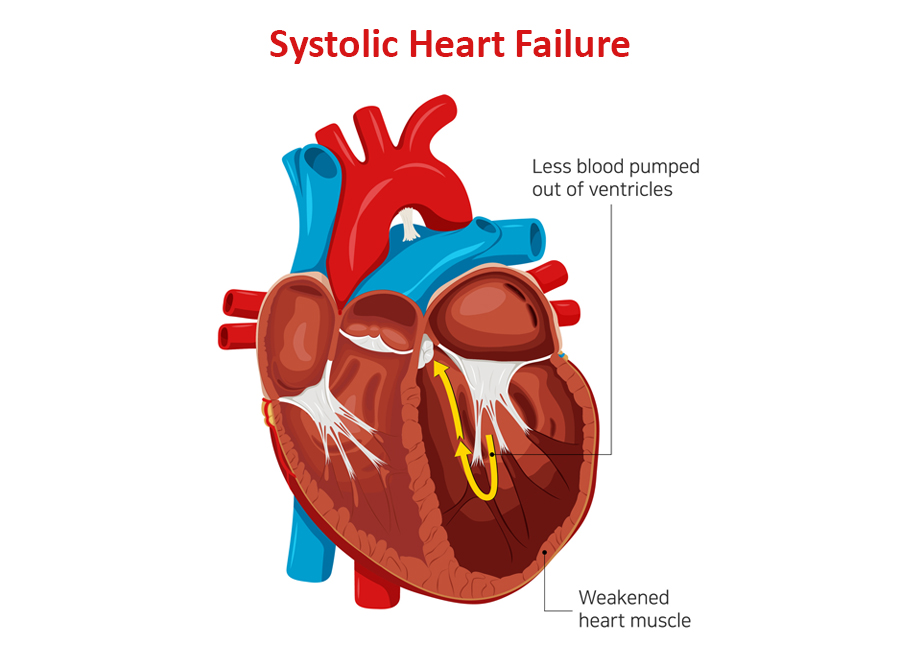
Systolic Heart Failure: A Closer Look
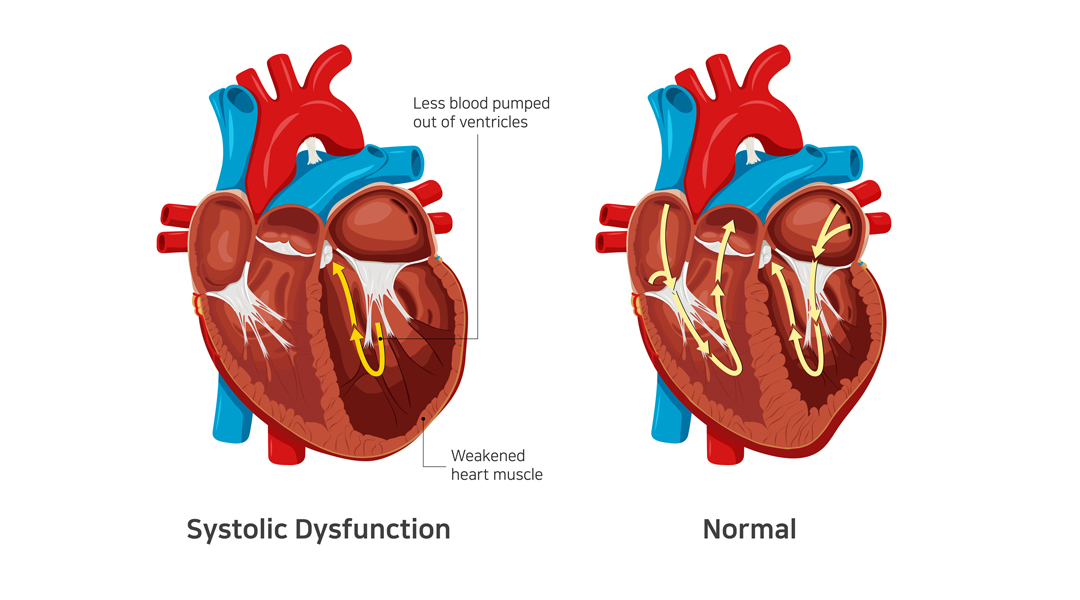
Systolic heart failure occurs due to a problem in the heart’s contraction (or systolic) phase. It’s characterized by stretching and weakening of the left ventricular muscle, due to which the heart pumps out less oxygenated blood to the body.
It’s also known as heart failure with reduced ejection infraction. As the condition worsens, it can also weaken the right ventricle and take a toll on its pumping power too.
Related: What Are the Symptoms of Diastolic Dysfunction?
Causes of Systolic Heart Failure
Systolic heart failure is caused by underlying medical conditions that damage the left ventricle. The most common causes include :
- Hypertension (the left ventricle has to use increased pressure to pump blood through the body)
- Coronary artery disease (buildup of cholesterol in the arteries) – with or without a heart attack.
- Dilated cardiomyopathy (weakening of the left ventricle due to an infection or long-term exposure to alcohol and narcotics)
- Abnormal heart rhythm (also known as atrial fibrillation)
- Previous heart attack
Additionally, people who are older or have diabetes are at a higher risk of developing systolic heart failure.
Related: Understanding Congestive Heart Failure Symptoms
Symptoms of Systolic Heart Failure
In systolic heart failure, an adequate amount of oxygen-rich blood doesn’t reach all organs. The most common indicator of the condition is a lower ejection fraction.
It can result in the following symptoms:
- Breathlessness – initially on exertion and in later stages even at rest or lying down.
- Swelling of feet, face, abdomen – due to fluid accumulation in various organs
- Engorged and pulsatile neck veins
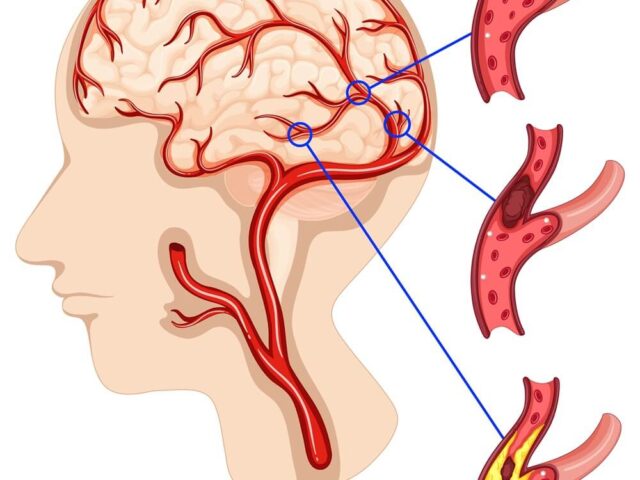
- Confusion (due to a lack of oxygen supply in the brain)
- Weight gain (due to a buildup of excess fluid in the body)
- Fatigue (due to reduced blood supply to the muscles)
- Pale or bluish skin tone (due to restricted blood supply to the skin and other vital organs).
Diagnosis and Treatment Options
Typically, a doctor prescribes various tests, such as chest X-ray, ECG, and echocardiography, to diagnose systolic heart failure and its root cause. The treatment plan depends on the underlying cause.
In most cases, systolic heart failure is treated using one or more of the following medications:
- Beta-blockers
- Diuretics or water pills
- ACE inhibitors
- Digoxin
- Anticoagulants
Additionally, doctors recommend a healthy diet and lifestyle changes to improve cardiac health and manage underlying conditions, such as hypertension and diabetes.
Related: Diagnosing Congestive Heart Failure
In Conclusion
If left untreated, systolic heart failure can damage vital organs and even lead to death. It’s crucial that patients watch out for symptoms like swollen feet, mental confusion, and bluish skin color and seek medical treatment at the earliest.
Dr. C Raghu is an experienced cardiologist who specializes in interventional cardiology and TAVR. If you or anyone you know is experiencing symptoms of systolic heart failure, connect with Dr. Raghu for proper diagnosis and treatment.
Book Online Consultaion
What Is Systolic Heart Failure ? – Blog
Subscribe the Hearty Life Blogs

DR. RAGHU | Best Cardiologist in Hyderabad
Cardiology Coronary, Vascular and
Structural Interventions
Conditions & Diseases
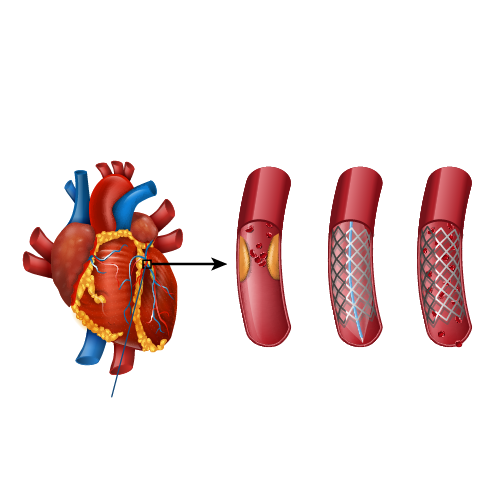
Angioplasty
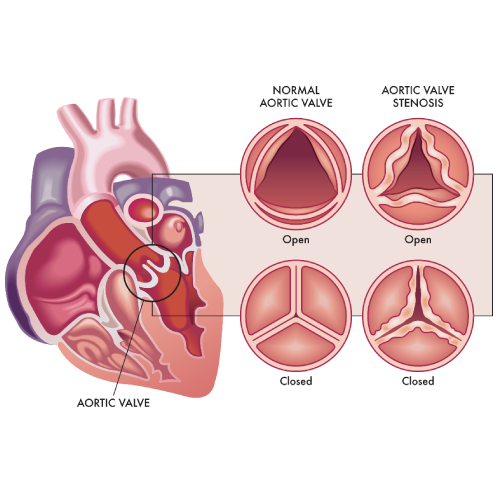
Aortic Stenosis
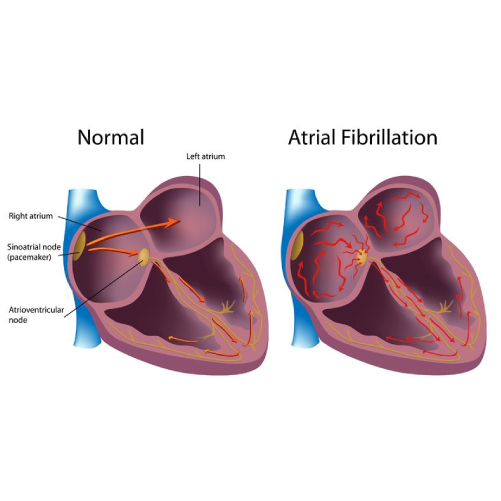
Atrial Fibrillation
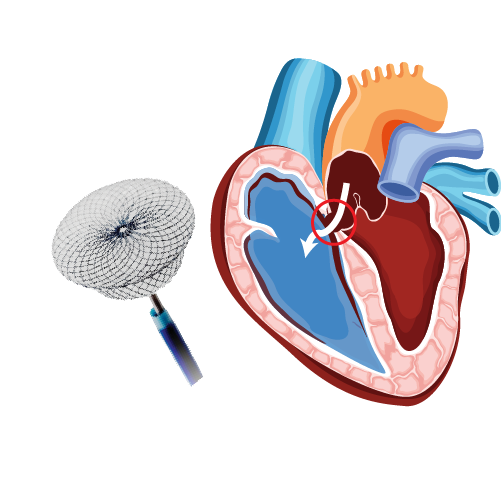
Atrial Septal Defect
ECG is a simple inexpensive test to asses heart function. ECG is the short form for electrocardiogram or electrocardiography.
Heart failure can be categorized into different types depending on various factors. While most conditions cause similar symptoms, clear identification of the type of heart failure is crucial for doctors to determine the proper course of treatment.