Heart failure is a condition in which the heart can’t pump enough blood to meet the body’s needs. It’s a serious condition that requires treatment by your doctor, but there are several options available.
Heart Failure | Dr Raghu
In our previous blogs, we’ve explored the causes, symptoms, and treatment options of heart failure. Also, we’ve outlined different types of heart failure in detail. You can click here to check out our previous blogs.
In this article, we’ll discuss left ventricular ejection fraction, one of the most common parameters doctors use to diagnose heart failure. Let’s dive right in.

What Is Ejection Fraction?
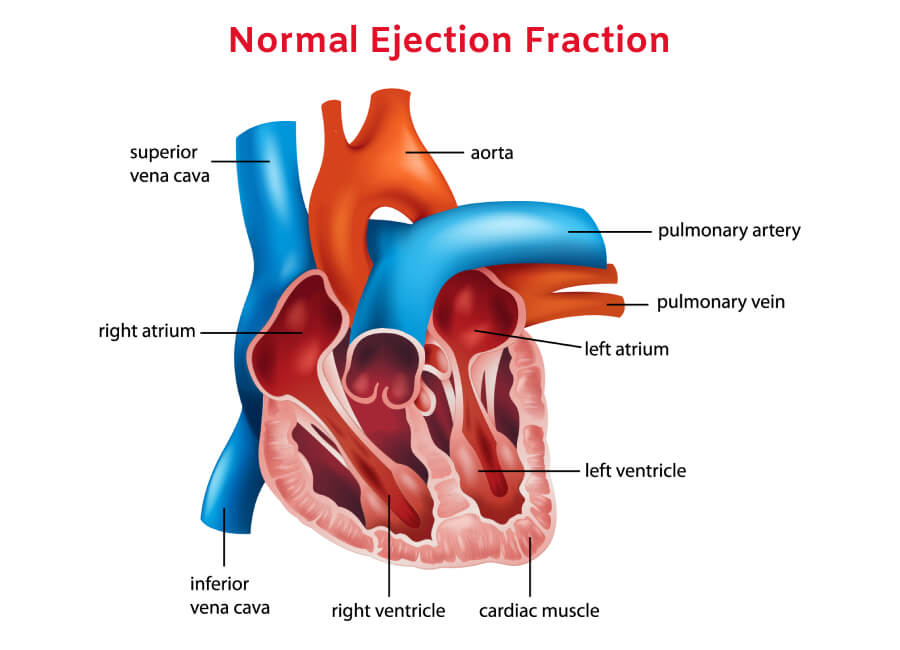
Simply put, ejection fraction is a measure of the amount of blood pumped out from the heart’s lower chambers (ventricles). Ejection fraction can be of two types:
- Left ventricular ejection fraction
- Right ventricular ejection fraction
Right ventricular ejection fraction is the percentage of deoxygenated blood the right ventricle pushes into the lungs. On the other hand, left ventricular ejection fraction (LVEF) is the percentage of oxygen-rich blood pumped out from the left ventricle into the arteries that carry blood to vital organs, muscles, and tissues.
Typically, doctors use the term “ejection fraction” when they refer to LVEF. If your heart is healthy and well functioning, the ejection fraction will range between 55% to 66%. An ejection fraction lower than 50% is a sign of systolic heart failure (or heart failure with reduced ejection fraction).
However, it’s possible for you to develop heart failure with an ejection fraction above 50%. In such cases, there’s a problem with the relaxed (or diastolic) phase of the heart’s pumping cycle. The condition is known as diastolic heart failure (or heart failure with preserved ejection fraction).
It’s worth noting that an abnormally high ejection fraction (above 70%) could be an indication of a heart condition like hypertrophic cardiomyopathy.
Symptoms of Low Ejection Fraction
As mentioned earlier, a low ejection fraction (below 50%) is a sign of heart failure. It means that the heart is unable to pump an adequate amount of blood into the arteries. It results in a shortage of blood supply to various organs. Also, it causes excess blood to back up in the lungs.
The most common symptoms of low LVEF include:
- Shortness of breath
- Mental confusion
- Pale or bluish skin color
- Swelling in the abdomen, feet, and legs
- Weight gain (due to fluid buildup)
- Loss of appetite
- Coughing and wheezing
Treatment of Low Ejection Fraction
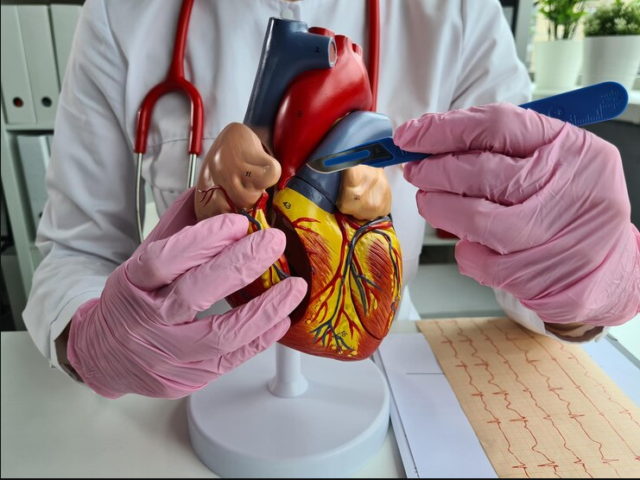
Cardiologists use a wide array of tests to detect a low ejection fraction and its underlying cause. These include ECG, echocardiogram, chest X-ray, etc. The course of treatment depends on the underlying disorder that’s causing low LVEF.
The most common treatment options include medications, such as digoxin (to strengthen the heart’s contractions), beta-blockers (to ease the heart’s workload), and diuretics (to minimize fluid buildup in the body).
Additionally, your doctor will recommend lifestyle changes, such as weight loss, exercise, and a healthy diet to improve LVEF. Also, it’s a good idea to avoid alcohol consumption and tobacco smoking.
In Conclusion
A low LVEF is a prominent sign of systolic heart failure. It can cause symptoms like shortness of breath and fluid buildup in the body. If you’ve been diagnosed with a low ejection fraction, consult your doctor to explore your treatment options.
Dr. C Raghu is an eminent cardiologist with years of experience. He specializes in interventional cardiology. If you or anyone you know is experiencing symptoms of heart failure, feel free to consult Dr. Raghu today.
Book Online Consultaion
Left Ventricular Ejection Fraction Blog
Subscribe the Hearty Life Blogs

DR. RAGHU | Best Cardiologist in Hyderabad
Cardiology Coronary, Vascular and
Structural Interventions
Conditions & Diseases

Angioplasty

Aortic Stenosis

Atrial Fibrillation

Atrial Septal Defect
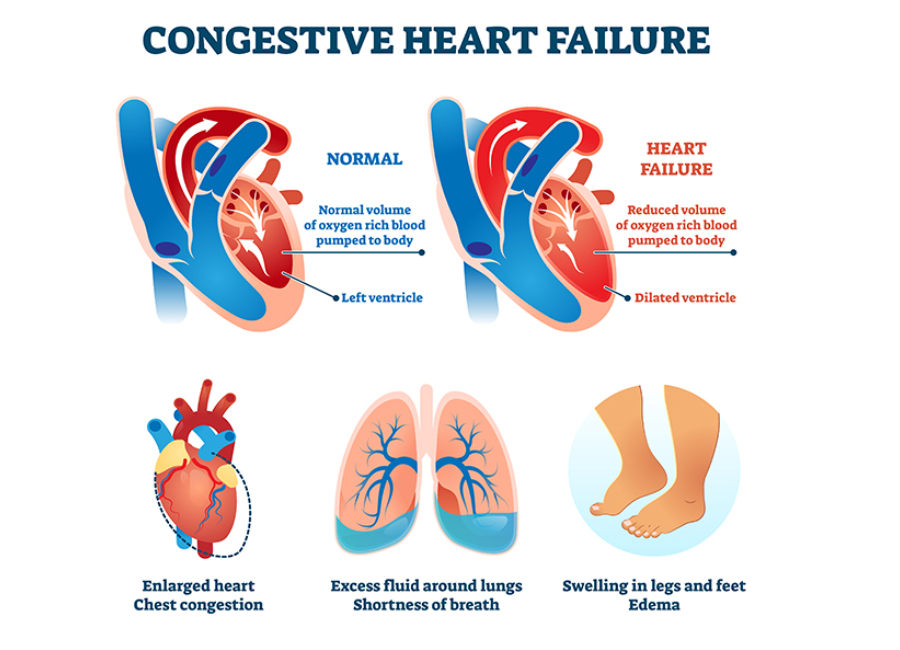
Heart failure is an umbrella term for a set of physical symptoms arising due to the gradual deterioration in the heart’s pumping ability. The term “congestive heart failure” was traditionally used because the condition resulted in fluid buildup and congestion in the lungs.
However, doctors and medical researchers have found that it causes a wide array of other symptoms. That’s why they now refer to the condition as heart failure.
What Happens in Congestive Heart Failure?
A healthy human heart relaxes and contracts nearly 100,000 times a day and pumps more than 2,000 gallons of blood throughout the body. The cardiovascular system also includes a network of arteries and veins to transport deoxygenated and oxygenated blood to and from the heart. If any part of the system falters, it can disrupt the flow of blood to vital organs.
Heart failure is characterized by a progressive decline in the heart’s power to pump blood. When that happens, the heart goes through a series of structural changes (knowns as cardiac remodeling) and beats faster to pump more blood.
Also, the blood vessels constrict to stabilize blood pressure and restrict blood supply to non-critical organs like the skin and kidneys. When blood flow to the kidneys reduces, it compels the body to retain more fluid and sodium.
All these short-term fixes result in more damage and cause even more stress to the heart muscles. That, in turn, results in further deterioration of the heart’s pumping action.
Congestive Heart Failure Symptoms: A Closer Look
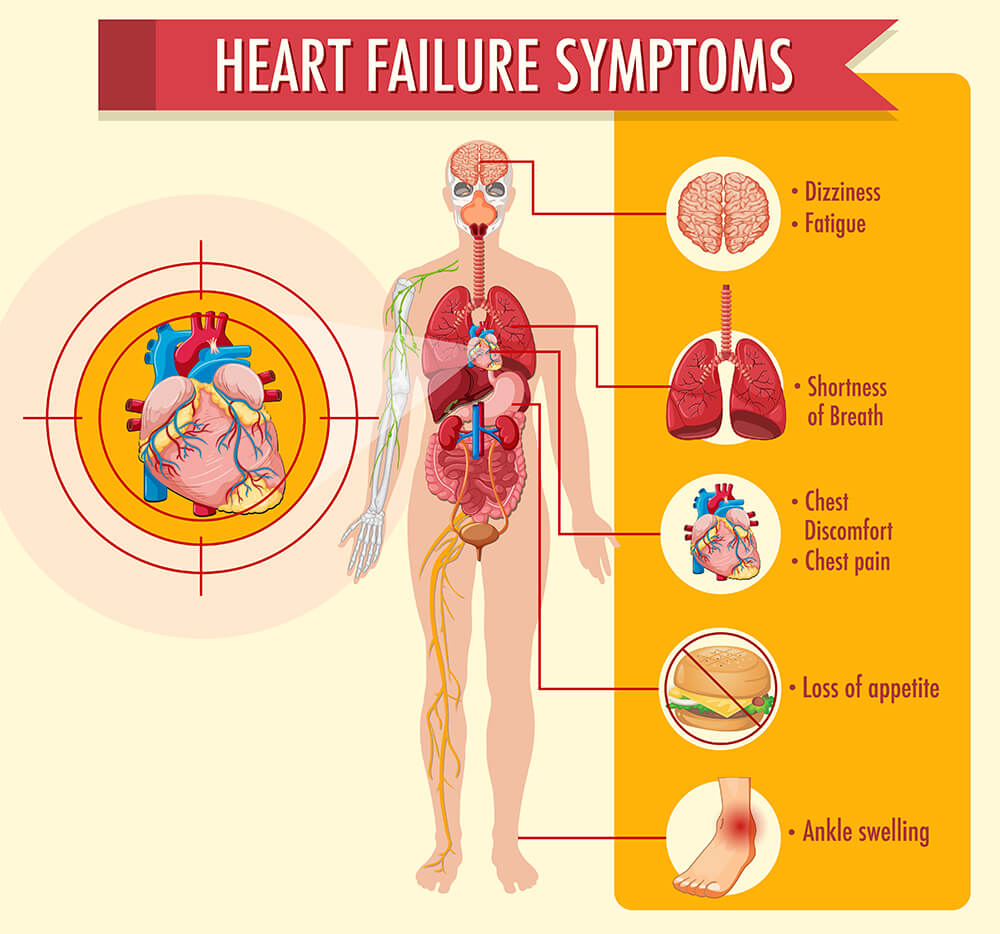
The heart failure symptoms vary depending on whether they’re caused due to a lack of oxygen or an increase in fluid build.
Lack of oxygen supply results in the following heart failure symptoms :
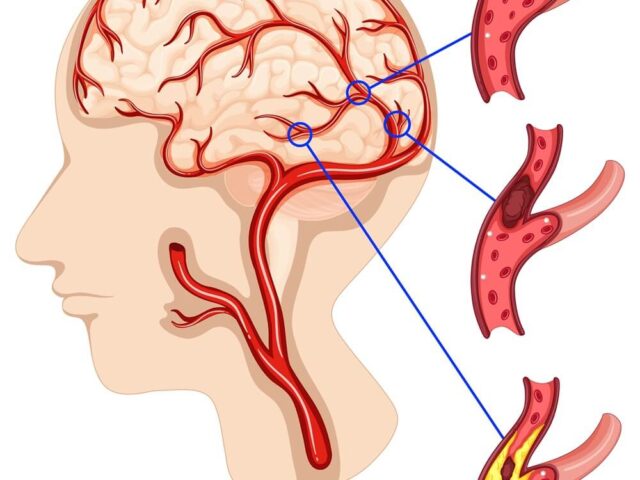
- Confusion
- Weight gain
- Fatigue
- Discolored or bluish skin
Excess sodium and fluid buildup in the body causes the following heart failure symptoms:
- Lung congestion
- Shortness of breath
- Coughing and wheezing
- Loss of appetite
- Swelling of feet and abdomen
Causes and Types of Congestive Heart Failure
The most common causes of heart failure include:
- Coronary artery disease (Narrowing of arteries due to cholesterol buildup)
- Damaged or dying heart tissue due to a heart attack
- Cardiomyopathy (damage to the heart muscles)
- Heart rhythm disturbances due to atrial fibrillation
- Underlying medical conditions like hypertension and diabetes
There are various ways to categorize congestive heart failure. Depending on the part of the heart’s pumping that’s affected due to heart failure, it can be of the following types:
- Systolic heart failure or heart failure with a reduced ejection fraction
- Diastolic heart failure or heart failure with a preserved ejection fraction
Also, depending on the side of the heart that’s affected, heart failure can be categorized as left-sided failure and right-sided failure. The treatment approach a doctor will use depends on the type of heart failure a patient has developed.
Stages of Heart Failure
The American College of Cardiology and the American Heart Association has outlined four stages to denote the progression of heart failure. While Stage A is characterized by risk factors like underlying medical conditions, stage B shows structural changes in a patient’s heart. The more advanced stages (C and D) present visible symptoms.
In Conclusion
Heart failure (also known as congestive heart failure) is a progressive condition caused by the heart’s inability to pump blood adequately. It results in symptoms like shortness of breath, fatigue, weight gain, and brain fog.
Dr. C Raghu is an eminent cardiologist with more than two decades of experience. If you or someone you know has developed congestive heart failure symptoms, consult Dr. Raghu to explore your treatment options.
Book Online Consultaion
Understanding Congestive Heart Failure Symptoms Blog
Subscribe the Hearty Life Blogs

DR. RAGHU
Cardiology Coronary, Vascular and
Structural Interventions
Conditions & Diseases

Angioplasty

Aortic Stenosis

Atrial Fibrillation

Atrial Septal Defect
Diagnosing heart failure involves a combination of physical examination, blood tests, and non-invasive procedures like X-rays and ECG.
In our previous articles, we’ve discussed the symptoms of heart failure and the steps to diagnose the same. However, the course of treatment varies for every patient based on the type of heart failure they’ve developed.
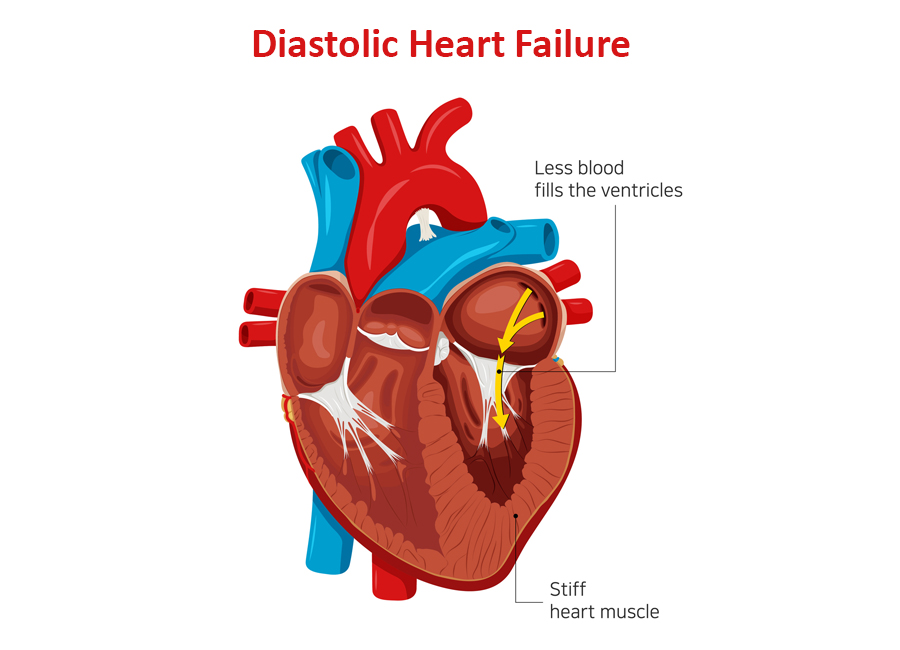
Depending on the part of the heart’s pumping cycle that’s been affected, there are two types of heart failure. In this blog, we’ll take a closer look at diastolic dysfunction and its symptoms.
What Causes Diastolic Dysfunction?
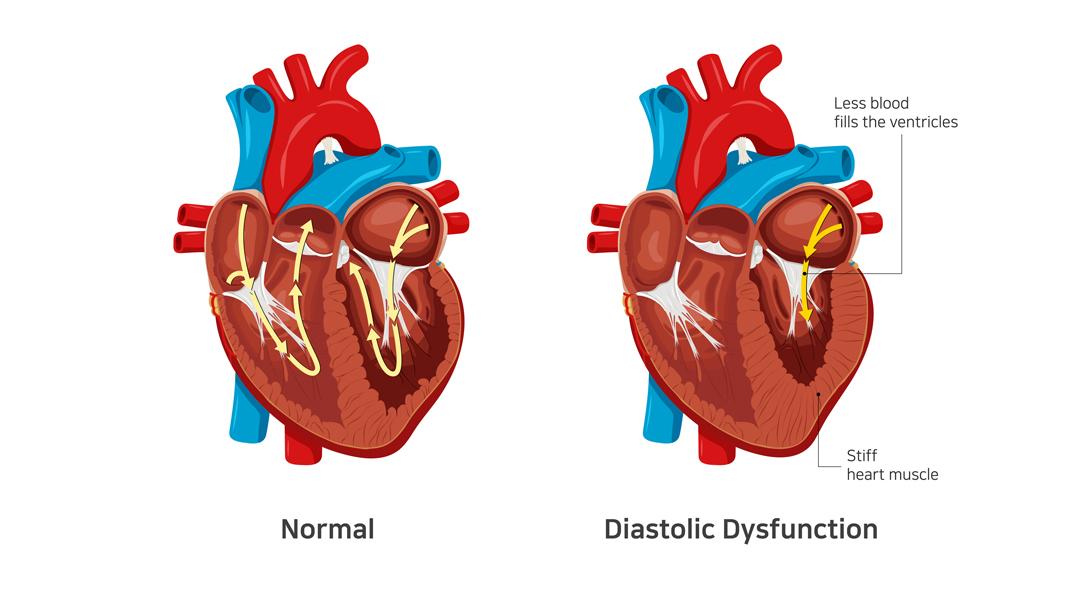
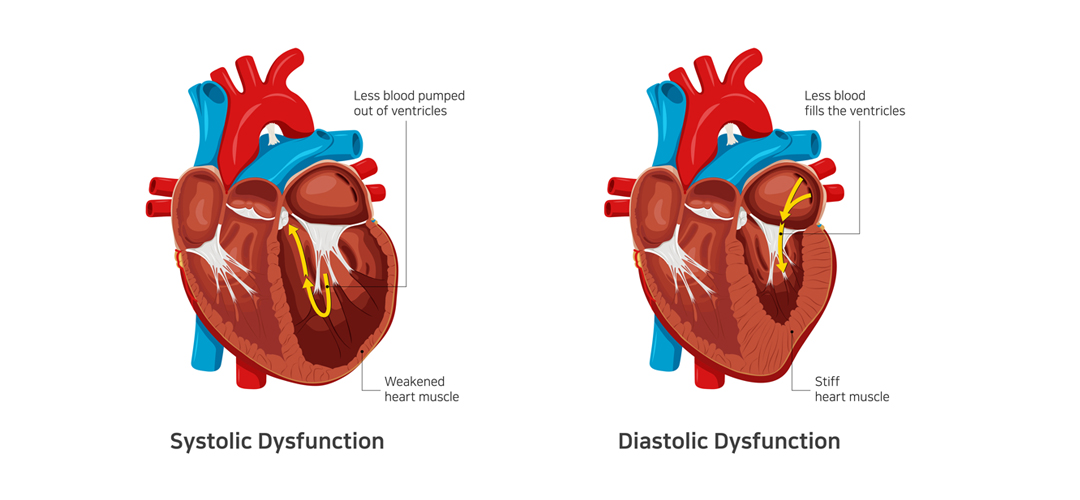
The diastolic phase refers to the part of the heart’s pumping cycle when the ventricles (lower chambers) relax and let blood flow in from the atria (upper chambers). Diastolic dysfunction is a condition in which the ventricles don’t relax enough. That, in turn, prevents the normal amount of blood from entering the heart.
Diastolic dysfunction is caused when the heart muscles become thicker and stiffer than usual. It’s more common in older women with hypertension and diabetes. If left untreated, it can lead to diastolic heart failure (also known as heart failure with preserved ejection fraction).
Related : Understanding Congestive Heart Failure Symptoms
What Does Preserved Ejection Fraction Mean?
Ejection fraction refers to the volume of blood pumped out from the heart’s left ventricle with each contraction. For a healthy heart, the number falls in the range of 55% to 65%. A lower ejection fraction is one of the most common indicators of heart failure.
However, it’s worth noting that many people with diastolic dysfunction have an ejection fraction of 50% or more (which is known as preserved ejection fraction). That means the left ventricle expels an adequate amount of oxygenated blood.
However, the heart muscle doesn’t relax enough to let a sufficient quantity of blood in. That, in turn, causes the excess blood to back up in the lungs and results in fluid buildup in the feet and abdomen.
How to differentiate systolic from diastolic dysfunction ?
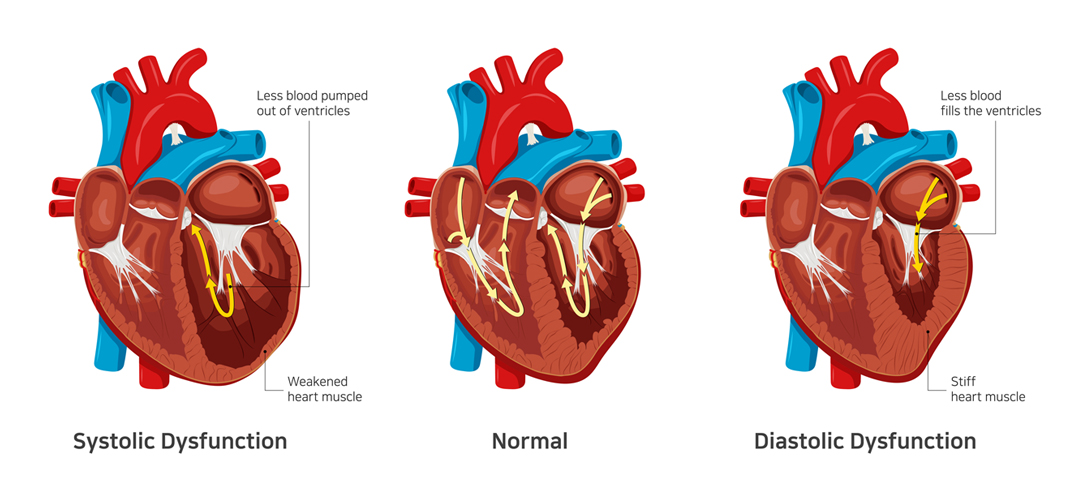
In contrast to systolic dysfunction where the heart muscle is “weak”, in diastolic dysfunction the heart is “stiff”. This means that the heart is unable to pump blood out of the heart in systolic dysfunction whereas the heart is unable to accept further blood in diastolic dysfunction. Both conditions lead to congestion or fluid accumulation in various organs of the body. Differentiation of heart failure from systolic and diastolic dysfunction is not possible as both diseases present with similar symptoms.
Which conditions lead to Diastolic dysfunction?
- Diastolic dysfunction appears consequent to uncontrolled or long-standing diabetes
- Hypertension
- Obesity as well as elderly people
- Women and atrial fibrillation
The best way to prevent and treat diastolic dysfunction is by effective control of the diseases mentioned above.
Symptoms of Diastolic Dysfunction
The most common symptom of diastolic dysfunction is congestion and shortness of breath due to the buildup of blood and fluid in the lungs. Breathing difficulties can get particularly worse during exertion or when lying.
Other symptoms of diastolic dysfunction include:
- Coughing and wheezing (due to lung congestion)
- Loss of appetite and nausea (due to fluid buildup around the liver and in the stomach)
- Swollen feet, legs, and abdomen (due to fluid accumulation)
If you experience any of the given symptoms, it’s crucial to consult a doctor for a proper diagnosis.
Treatment of Diastolic Dysfunction
Treatment of diastolic dysfunction involves a combination of medications (diuretics or water pills) and lifestyle changes. In severe cases, a patient might need left ventricular assist devices or a heart transplant.
Is Diastolic Dysfunction Serious?
In the long run, diastolic dysfunction can lead to diastolic heart failure. That, in turn, increases your risk of hospitalization and death. Therefore, you should pay close attention to your symptoms and reach out to a doctor whenever you notice anything unusual.
Dr. C Raghu is a renowned cardiologist who specializes in interventional cardiology. He has decades of experience in treating patients with different heart conditions. If you or anyone you know has developed symptoms like shortness of breath, swollen feet, loss of appetite, etc., contact Dr. Raghu to explore your treatment options.
Book Online Consultaion
What Are the Symptoms of Diastolic Dysfunction ? – Blog
Subscribe the Hearty Life Blogs

DR. RAGHU | Best Cardiologist in Hyderabad
Cardiology Coronary, Vascular and
Structural Interventions
Conditions & Diseases

Angioplasty

Aortic Stenosis

Atrial Fibrillation

Atrial Septal Defect
Congestive heart failure is characterized by a gradual deterioration in the heart’s ability to pump blood throughout the body. It can result in various symptoms, such as swelling in the abdomen, feet, and legs, shortness of breath, fatigue
Heart failure refers to a condition where the heart is unable to pump blood throughout the body with maximum efficiency. It’s usually the result of progressive weakening, thickening, or stiffening of the heart muscles.
Heart failure is a common condition with no known cure. However, proper treatment can control the disease progression and thus improve a patient’s quality of life and longevity. To decide the proper course of treatment, a doctor must first determine the type of heart failure a patient has developed.
Depending on the part of the heart’s pumping cycle that’s been affected, heart failure can be of two types – diastolic and systolic. You can learn more about the symptoms, causes, treatment of diastolic dysfunction and differentiation from systolic dysfunction in our previous article.
In this blog, we’ll delve deeper into systolic heart failure and understand its causes and symptoms.
Systolic Heart Failure: A Closer Look
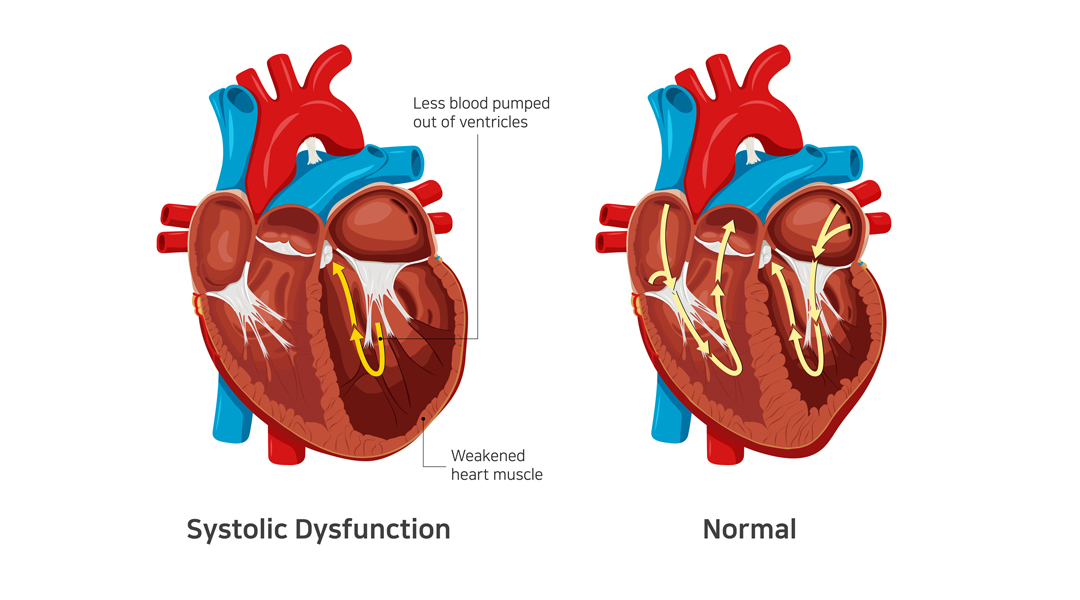
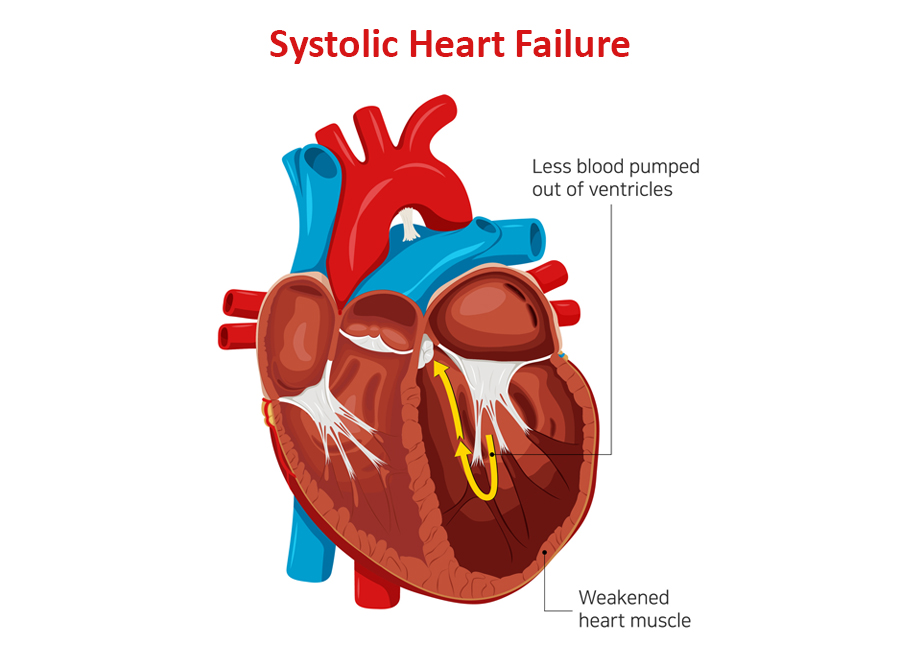
Systolic heart failure occurs due to a problem in the heart’s contraction (or systolic) phase. It’s characterized by stretching and weakening of the left ventricular muscle, due to which the heart pumps out less oxygenated blood to the body.
It’s also known as heart failure with reduced ejection infraction. As the condition worsens, it can also weaken the right ventricle and take a toll on its pumping power too.
Related: What Are the Symptoms of Diastolic Dysfunction?
Causes of Systolic Heart Failure
Systolic heart failure is caused by underlying medical conditions that damage the left ventricle. The most common causes include :
- Hypertension (the left ventricle has to use increased pressure to pump blood through the body)
- Coronary artery disease (buildup of cholesterol in the arteries) – with or without a heart attack.
- Dilated cardiomyopathy (weakening of the left ventricle due to an infection or long-term exposure to alcohol and narcotics)
- Abnormal heart rhythm (also known as atrial fibrillation)
- Previous heart attack
Additionally, people who are older or have diabetes are at a higher risk of developing systolic heart failure.
Related: Understanding Congestive Heart Failure Symptoms
Symptoms of Systolic Heart Failure
In systolic heart failure, an adequate amount of oxygen-rich blood doesn’t reach all organs. The most common indicator of the condition is a lower ejection fraction.
It can result in the following symptoms:
- Breathlessness – initially on exertion and in later stages even at rest or lying down.
- Swelling of feet, face, abdomen – due to fluid accumulation in various organs
- Engorged and pulsatile neck veins
- Confusion (due to a lack of oxygen supply in the brain)
- Weight gain (due to a buildup of excess fluid in the body)
- Fatigue (due to reduced blood supply to the muscles)
- Pale or bluish skin tone (due to restricted blood supply to the skin and other vital organs).
Diagnosis and Treatment Options
Typically, a doctor prescribes various tests, such as chest X-ray, ECG, and echocardiography, to diagnose systolic heart failure and its root cause. The treatment plan depends on the underlying cause.
In most cases, systolic heart failure is treated using one or more of the following medications:
- Beta-blockers
- Diuretics or water pills
- ACE inhibitors
- Digoxin
- Anticoagulants
Additionally, doctors recommend a healthy diet and lifestyle changes to improve cardiac health and manage underlying conditions, such as hypertension and diabetes.
Related: Diagnosing Congestive Heart Failure
In Conclusion
If left untreated, systolic heart failure can damage vital organs and even lead to death. It’s crucial that patients watch out for symptoms like swollen feet, mental confusion, and bluish skin color and seek medical treatment at the earliest.
Dr. C Raghu is an experienced cardiologist who specializes in interventional cardiology and TAVR. If you or anyone you know is experiencing symptoms of systolic heart failure, connect with Dr. Raghu for proper diagnosis and treatment.
Book Online Consultaion
What Is Systolic Heart Failure ? – Blog
Subscribe the Hearty Life Blogs

DR. RAGHU | Best Cardiologist in Hyderabad
Cardiology Coronary, Vascular and
Structural Interventions
Conditions & Diseases

Angioplasty

Aortic Stenosis

Atrial Fibrillation

Atrial Septal Defect
The ejection fraction is one of the most common parameters used to diagnose heart failure. If you want to know more about the cause, symptoms, and types of heart failure, check out our previous blog posts.
The most likely cause of right sided heart failure is a weak left ventricle. In other words, left sided heart failure eventually leads to right sided heart failure.