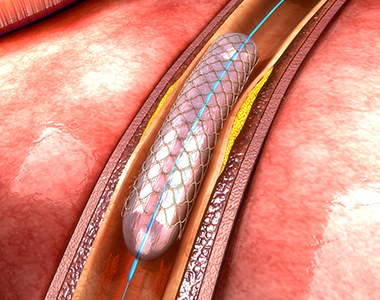
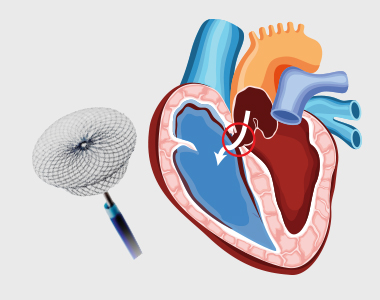
Coronary arteries are the blood vessels that delivers oxygenated blood to the heart muscle. But, sometimes these blood vessels may get narrowed or blocked due to accumulation of cholesterol plaque. To open the blockage and restore the function of arteries, coronary angioplasty is performed.
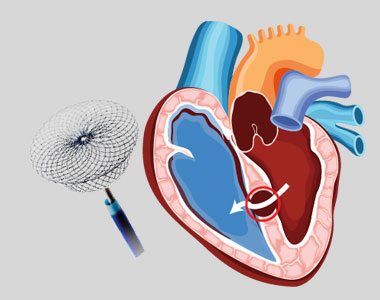
A coronary angioplasty involves the temporary insertion of a tiny balloon inside the artery to open the blockage. It is usually combined with the placement of a stent (a metal mesh tube) to widen the artery and prevent the further chance of narrowing.

Why is coronary angioplasty done ?
Coronary angioplasty is done to treat narrowing or blockage of the heart’s blood vessels:
- during or after a heart attack.
- Blood vessel narrowing leading to poor heart function.
- For relief of chest pain (angina) due to reduced blood supply to heart.
Risks of coronary angioplasty
Usually, it is a safe procedure, but like all other procedures, it also carries certain risks like:
| Common Issues/Risks after angiography | |
|---|---|
| Bruising | Common to have bruise at groin or arm Lasts for few weeks Not to be worried about |
| Allergic reactions | Usually related to contrast medicine used History of previous allergy – higher risk Present as rash and headache |
| Bleeding at the site of entry (Hematoma) | Usually subsides in a few days But in case swelling is increasing and painful contact your physician immediately |
| Serious complications after coronary angiography | Less than 1 in 1000 chance People with severe heart disease are at high risk Discuss with Cardiologist before procedure |
|---|---|
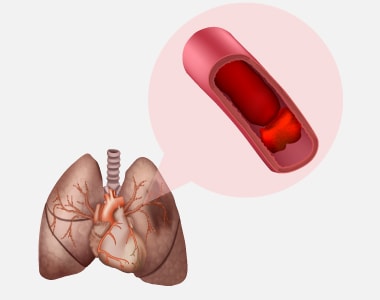
| Heart attack | A serious medical emergency where the heart’s blood supply is suddenly blocked |
| Stroke | A serious medical condition that occurs when the blood supply to the brain is interrupted |
| Loss of blood supply to limb | Damage to the artery in the arm or groin in which the catheter was inserted, with the blood supply to the limb possibly being affected |
| Kidney injury | Damage to the kidneys caused by the contrast dye |
| Radiation injury | Tissue damage caused by X-ray radiation if the procedure is prolonged |
What happens before the procedure?
A physical examination and blood test are done to evaluate the overall health condition. The person needs to follow instructions provided before undergoing the procedure:
1. Inform the doctor about:
- Any allergies
- The use of current medicines, including vitamin and mineral supplements
- Any blood disorder
- Any surgery you may had
- The past and present medical condition
2. Medicines:
Tell the doctor if you are using blood thinners or any anti-diabetic medicines. The doctor will either advise you to stop or change the dose of the medication.
3. Food and fluid restrictions:
- Avoid heavy meals, such as meat, fried or fatty foods eight hours before the procedure. Take light foods such as toast and cereal.
- Fast for six hours before the procedure.
- Stay hydrated, drink plenty of fluid up to two hours before the procedure.
In most of the cases, you will be discharged on the same day of the hospital, so ask someone to accompany you to the hospital.