Coronary arteries are the vessels which supply blood (oxygen and nutrients) to the heart; this supply may be disrupted due to buildup of cholesterol and fatty deposits, called plaques, on the inner walls of the arteries (atherosclerosis) causing narrowing of the vessel lumen.
Coronary lesions branch out as they progress to supply various cardiac structures. A bifurcation lesion is a stenosis or abnormal narrowing of greater than 50% that occurs in a coronary artery at the origin of the side branch or adjacent to the origin of the side branch. Branching points a.k.a bifurcation points in the coronary arteries are prone to develop atherosclerosis as the shear stress is higher at the branch points.
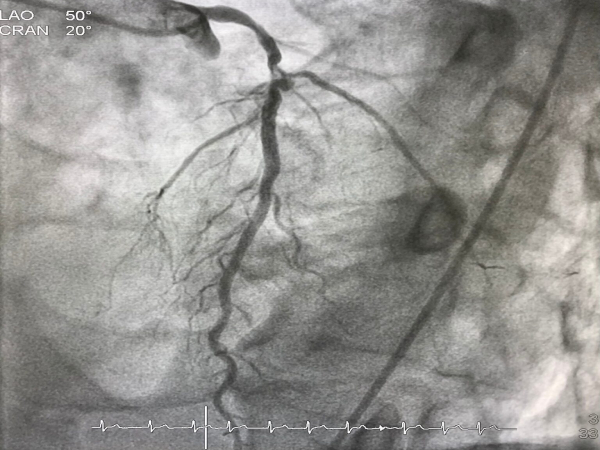
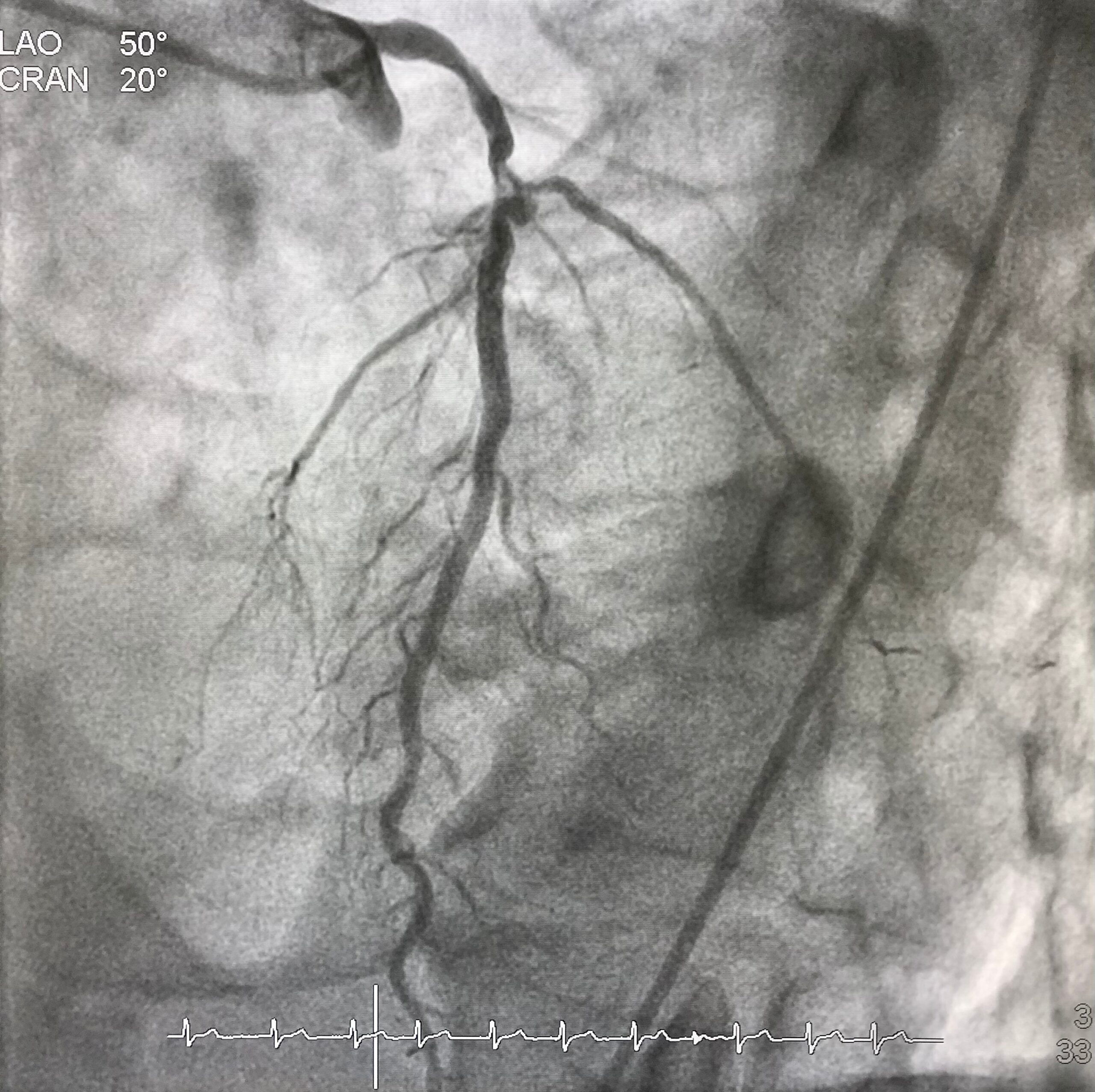
The figure shows how a bifurcation stenosis appears schematically as well as on angiography.
Why bifurcation lesions are important?
A vast majority of coronary arteries obstructions happen at the branching point. About 15-20% of patients of referrals for bypass surgery are because of the presence of coronary narrowing at bifurcation location. They are considered a tough lesion to treat by angioplasty and stent.
How are bifurcation lesions diagnosed?
Bifurcation lesions are identified on coronary angiography. Only lesions affecting side branch blood vessels more than 2.25 mm is considered important and called bifurcation lesions. The main vessel that gives branches is called main vessel and the branches that originate from it are called side branches. The point at the division of the main vessel and side branch is called a bifurcation point.
How is a bifurcation lesion unique?
Bifurcation lesions can involve the coronary artery either before or after the bifurcation point. In addition, side branches could be either diseased or free from disease. Based on the location and severity of the cholesterol plaque at the bifurcation point, sub types of bifurcation lesions have been identified.
The challenge of performing angioplasty and stent for a bifurcation stenosis lies in the ability to preserve the main vessel and the side branch. Stents being metallic tubes risk occluding the side branch when placed across the side branch. This apprehension of losing the side branch, is one of the primary reasons for patients to be sent for bypass surgery instead of angioplasty and stent.

Can angioplasty and stent be performed for a bifurcation lesion?
Angioplasty and stent can be eminently performed for a bifurcation stenosis. Over the last 2 decades numerous techniques in stent implantation have been developed to treat the bifurcation lesions. Some of these techniques include:
- Provisional T stent technique
- Tap technique
- Double kiss crush technique
- Culotte technique
Advent of these techniques enabled experienced operators to perform angioplasty and stent successfully with chances of repeat narrowing seen in 3-6% patients at the site of stenting. Risk of losing a side branch after stenting is reduced to 1% once the new techniques are employed.
Dr. C Raghu is an expert in bifurcation lesion angioplasty and the center where he has been trained, ICPS Paris France is considered the “Mecca” for bifurcation lesion angioplasty techniques development.
How does a bifurcation lesion angioplasty differ from a normal angioplasty?
Bifurcation lesion angioplasty, involves utilization of novel stent techniques mentioned above. In addition, angioplasty operator experience is a major factor in determining outcomes. Choosing the “right” stent that allows side branch access, use of specialized technologies such as fractional flow reserve (FFR), expertise in deploying 2 stents especially the process of “stent crush” and the handling of two balloons through a single catheter – kissing balloon are key points for the best results in a stent procedure.
What are the chances of side branch occlusion in a bifurcation lesion angioplasty?
Contemporary bifurcation angioplasty using Intravascular imaging employing contemporary stenting techniques in the hands of expert bifurcation angioplasty operators carries a 99% success rate with a chance of losing side branch in 1% and repeat narrowing at the end of 9 months being 3-6%. These results are comparable and if not superior to bypass surgery as angioplasty entails a short hospital stay and fast recovery.