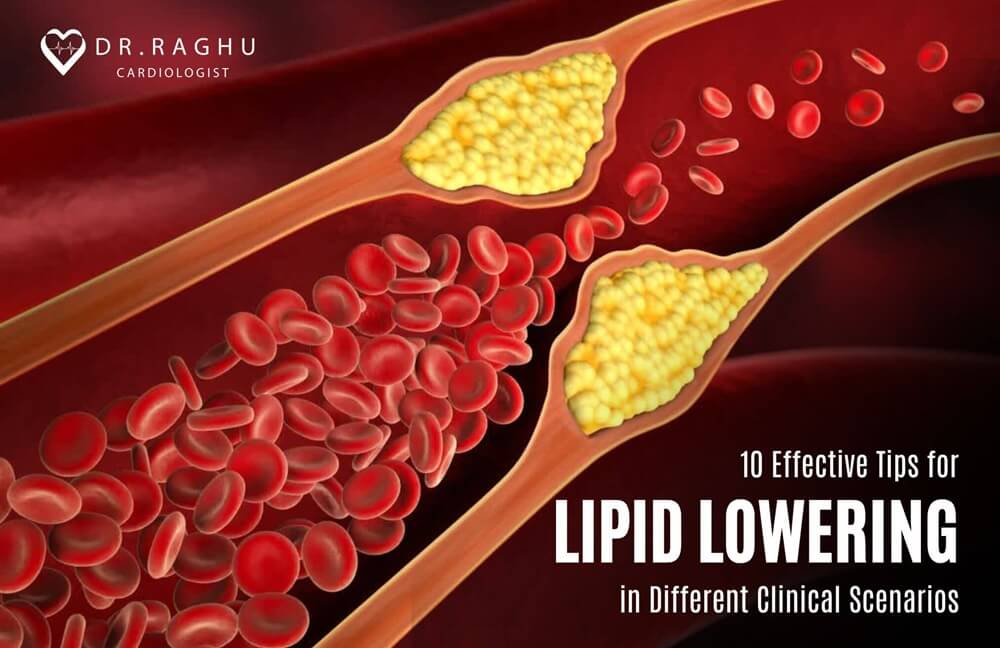
Cardiovascular health is intricately linked to lipid management, and effective strategies for lipid-lowering play a pivotal role in preventing cardiovascular diseases.
hypertension | Dr Raghu
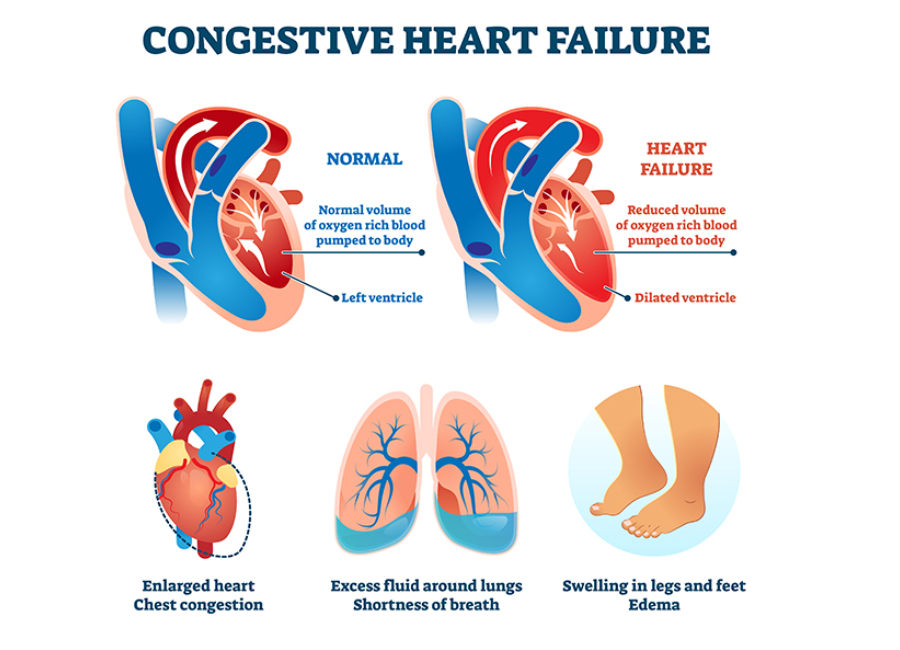
Heart failure is a chronic and progressive condition that occurs when the heart cannot pump blood efficiently to meet the body’s demands. As one of the leading causes of hospitalization worldwide, managing heart failure is crucial for improving patient outcomes and quality of life. One essential aspect of heart failure management is pacing, a therapeutic approach that involves the use of electronic devices to regulate the heart’s rhythm.
In this article, we will explore the significance of pacing in heart failure, the types of pacing devices available, and their role in enhancing patient well-being.
Understanding Heart Failure
Before delving into the intricacies of pacing, it’s essential to grasp the basics of heart failure. This condition can result from various underlying causes, such as coronary artery disease, hypertension, or cardiomyopathy. As the heart weakens, it struggles to pump blood effectively, leading to symptoms like shortness of breath, fatigue, and fluid retention. The severity of heart failure is often classified into stages, ranging from mild to advanced, with pacing becoming a viable intervention in more advanced cases.
The Role of Pacing in Heart Failure Management
Pacing is a therapeutic strategy employed to regulate the heart’s rhythm and improve its pumping efficiency. In heart failure, abnormal heart rhythms (arrhythmias) can exacerbate the condition, leading to further deterioration. Pacing devices, such as pacemakers and implantable cardioverter-defibrillators (ICDs), are designed to address these issues by ensuring the heartbeats are coordinated and synchronized.
Different types of pacing devices used in heart failure treatment include:
Pacemakers
Pacemakers are small, implantable devices that regulate the heart’s rhythm by sending electrical impulses to the heart muscles. They are commonly used in cases where the heart’s natural pacemaker (the sinoatrial node) is unable to maintain a regular rhythm. Pacemakers can be further categorized into single-chamber, dual-chamber, or biventricular pacemakers, each serving specific purposes based on the patient’s condition.
Implantable Cardioverter-Defibrillators (ICDs)
ICDs are advanced pacing devices equipped with additional capabilities. In addition to pacing functions, ICDs can detect and terminate potentially life-threatening arrhythmias by delivering electrical shocks to restore a normal heart rhythm. This is particularly crucial in heart failure patients at risk of sudden cardiac death due to ventricular arrhythmias.
Cardiac Resynchronization Therapy (CRT) Devices
CRT devices, also known as biventricular pacemakers, are specifically designed for heart failure patients with impaired ventricular function. These devices synchronize the contractions of the heart’s ventricles, improving overall cardiac performance. CRT is often recommended when heart failure symptoms persist despite optimal medical therapy.
Clinical Considerations and Patient Selection
Pacing is not a one-size-fits-all solution, and careful consideration is required when determining the appropriateness of pacing devices for heart failure patients. Factors such as the underlying cause of heart failure, the severity of symptoms, and the presence of arrhythmias play a crucial role in the decision-making process. A thorough evaluation by a cardiac electrophysiologist is essential to identify the most suitable pacing strategy for each patient.
Benefits and Outcomes of Pacing Devices
Pacing devices offer significant benefits in the management of heart failure, contributing to improved patient outcomes and a better quality of life. Firstly, these devices, such as pacemakers, help regulate the heart’s rhythm, ensuring coordinated contractions that enhance cardiac efficiency.
This is vital in heart failure, where irregular heart rhythms can worsen the condition. Secondly, pacing devices improve cardiac output by optimizing heart function, leading to increased blood flow and meeting the body’s oxygen and nutrient demands more effectively.
Moreover, the use of pacing devices has been associated with a reduction in heart failure symptoms, including fatigue, shortness of breath, and exercise intolerance. By enhancing the heart’s pumping capacity, patients often experience an alleviation of these debilitating symptoms, leading to an overall improvement in well-being.
Pacing devices, particularly implantable cardioverter-defibrillators (ICDs), also play a crucial role in preventing life-threatening arrhythmias, reducing the risk of sudden cardiac death in heart failure patients.
Additionally, the impact of pacing devices extends to a broader improvement in the quality of life for heart failure patients. These devices, through advancements in technology and tailored treatment approaches, allow for a personalized management strategy.
Conclusion
Pacing has emerged as a valuable tool in the comprehensive management of heart failure, offering tailored solutions to address rhythm abnormalities and enhance cardiac function. As technology continues to advance, ongoing research and innovation in pacing devices hold the promise of further improving outcomes for heart failure patients.
With a multidisciplinary approach involving healthcare providers, cardiac electrophysiologists, and patients, pacing remains a vital component in the arsenal against this challenging cardiovascular condition.
Dr. C Raghu is a renowned cardiologist based out of Hyderabad. He specializes in interventional cardiology and has helped countless patients live longer healthier lives. If you or anyone you know is looking for heart disease treatment, reach out to Dr. Raghu today.
Book Online Consultaion
Understanding Pacing in Heart Failure Management: A Comprehensive Guide
Subscribe the Hearty Life Blogs

DR. RAGHU | Best Cardiologist in Hyderabad
Cardiology Coronary, Vascular and
Structural Interventions
Conditions & Diseases

Angioplasty

Aortic Stenosis

Atrial Fibrillation

Atrial Septal Defect
The COVID-19 pandemic brought to light the delicate connection between various pre-existing health conditions and the severity of the disease caused by the SARS-CoV-2 virus. Hypertension has emerged as a significant contributor to the development of severe COVID-19 among these conditions.

Hyderabad, July 9 (IANS) Vitamin D deficiency is not a major risk factor for heart attacks or atrial fibrillation. It is a soft target and not a hard point in management of heart disease, opines leading cardiologist Dr C. Raghu. According to him, the major risk factors for heart attacks remain hypertension, diabetes, high cholesterol and family history
In an interview with IANS, the senior interventional cardiologist and clinical director at Yashoda Hospitals, Secunderabad, explained some of the recent advances in the domain of heart heath.
Q: How do you look at the recent study that Vitamin D might reduce the risk of heart attacks and prevent irregular heartbeats?
A: These are not therapies for these problems. These are in addition to what all other measures a person takes. People might think that Vitamin D is the only thing. Heart disease is a multi-factor disorder.
Still, the standard risk factors remain diabetes, hypertension, high cholesterol and family. These have strong correlation. Vitamin D to treat or to prevent heart attack is still a long term goal even going by this study.
Many studies might come on various factors and they might choose positive benefits but for these positive benefits to translate to clinical medicine is a long process.
There are many medications which can definitely reduce the heart event rate but for this many factors have to be addressed properly.
Vitamin D is a very soft target not a hard point. It is not the only thing. People should not think that if I take Vitamin D, I will be okay. I think fundamentals remain the same.
Diabetes, hypertension, high cholesterol and physical activity continue to remain major pillars. These risk factors have to be addressed to prevent heart attack.
Q: How common is atrial fibrillation in the Indian context?
A: Atrial fibrillation is worsening like heart disease. It is a multifactorial disease. Most of the patients of atrial fibrillation are elderly women they have underlying hypertension, diabetes and they have stiff heart syndrome. In this group of patients prone to develop atrial fibrillation there are many hard end points which we can address rather than focusing on Vitamin D.
Vitamin D is not a major risk factor. In the Indian context also, atrial fibrillation is an emerging epidemic.
The main reasons are still uncontrolled high blood pressure, aging process and stiff heart. These will continue to be the main promoters of development atrial fibrillation. As a doctor, I would prefer to treat them rather than treat a very soft end point like Vitamin D.
Q: Will the use of higher doses of Vitamin D for a longer period negatively impact patients? If yes, what are the risks?
A: Yes. That is one of the major reasons why one should be very careful. Somebody might think what is the harm in consuming Vitamin D as it is a simple medication but that’s not the way. Unsupervised Vitamin D use for a prolonged period of time can lead to lot of medical complications.
Some people might develop renal dysfunction, some people might develop hyperparathyroidism or produce more calcium (hypercalcemia). There are a lot of metabolic problems that may happen if somebody takes long duration vitamin D without proper medical supervision.
Presence of deficiency of Vitamin D and its correction are not the same. Sometimes correction of vitamin D deficiency might not reduce the primary problem. Prolonged consumption of Vitamin D and unsupervised especially elderly people tend to develop more complications.
One should be cautious in taking Vitamin D without supervision. Having said that, there are a lot of natural sources for production of Vitamin D. I would prefer my patients to have a natural way to produce Vitamin D by their body as a medication.
I encourage my patients to have 15 minutes of sunlight at least 2-3 times a week and at least once a week, do traditional remedies like application of castor oil to promote internal development of Vitamin D. These are simple measures one can take and naturally produce Vitamin much more quantitatively better.
Q-What are the other new or recent discoveries for managing heart health?
A: In the management of heart health, what the recent advances suggest is to stick to the traditional risk factors only. We now have a lot of objective data.
Let us consider Lipid. We have a lot of data which emerged in the last one decade indicating that people should target their Lipid. There is a lot of misinformation and misconception which are being propelled by various sources indicating that one should not believe in Lipid but we have strong data on the management of Lipid.
We have clear-cut numbers. What is LDL cholesterol a person should have. The numbers are different for a person who does not have heart attack and the one who had heart attack.
For a person who does not have a heart attack but has only Diabetes, we aim for LDL of less than 70. Same for a person with heart attack we aim for LDL cholesterol of less than 55. Same for a person who has got a high risk we aim for less than 35.
Previously we never used to aim for such low levels of LDL cholesterol. Now we understand that a very low level of LDL cholesterol will reduce the risk of having a cardiac event. This is one of the important advances which I think people have to be aware of.
There are different cut-off levels. When people go to a laboratory, the normal value of cholesterol creates confusion.
They will try to remain at a much higher level than what is desired for them. A lot of personalised medicine is coming for different subsections of people. It might look very less interesting for people but it is a very important and also inexpensive way to reduce the risk of heart attack.
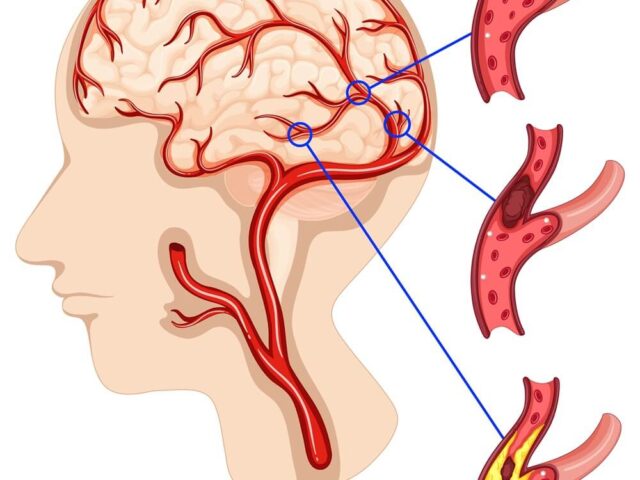
One of the common ways to reduce heart attacks is to use aspirin. We all think that taking aspirin a day reduces the risk. Now with the availability of new data, we can understand that certain groups of patients get benefited and certain groups of patients can get harmed.
What we understand is that aspirin used for patients less than 60 who have diabetes and hypertension, they get better whereas for patients who are more than 60 years, we have to select patients who are going to be benefited rather than using aspirin for all of them as a blanket.
Aspirin therapy is very useful for prevention of heart stroke in people who already had a heart attack but for those people who never had a heart attack in the past or who never had bypass surgery, it is better to limit the use of aspirin among people who are less than 60.
So we have to differentiate between those who had heart attack angioplasty vis-a-vis those who never had an event and use aspirin selectively for people who already had heart attack and for those who did not have heart attack, we need to calculate the risk and then only use benefit of the therapy.
We now understand that women tend to have a higher risk of heart attack than what we were thinking in the past. Now a days, we see a lot of women also developing heart attacks. That is due to multiple to new risk factors which we were hitherto not knowing.
These risk are enhancers: for women who tend to premature menopause naturally or surgically, they will have a higher risk of heart attack. Premature means less than 40.
Women who have immunological disorders like Rheumatoid arthritis or SLE tend to have higher chances of heart attack. Such women possibly take aspirin to prevent heart attack.
In addition to traditional risk factors, we have risk enhancing factors for women and people who have South Asian ancestry like Indians. They play an important role for the development of heart attacks.
South Asian ancestry people tend to have higher risk of heart attack especially those with a family history of heart attacks in less than 50 years of age. Those people are at higher risk of developing heart attacks. That is also considered a risk enhancer.
That’s why you see a lot of young people developing heart attacks among the Indian population because of our propensity. It is not considered as risk factor but considered risk enhancer
Compared to the past we are seeing more and more women developing heart attacks at younger age. Previously we were not seeing this. Women who tend to have higher blood pressure during pregnancy may develop heart attacks. This is also considered a risk enhancer for a heart attack.
Q: Is building more data helping understand the risk factors and risk enhances better?
A: We continue to get data. The larger the data set, better we can understand the association.
Risk scores have also been developed. These risk scores help us to estimate what is the risk of a particular person to a heart attack in the next 10 years. With these risk scores, objective risk assessment is possible compared to what we used to assess risk in a subjective way.
For the Indian population who are having a risk of more than 10 per cent, it is considered high risk in India. This means more than 10 per cent chance of having a heart attack in the next 10 years is considered high risk in India.
Indian race and south Asian ancestry itself is a risk enhancer. If risk calculation is more than 10 per cent, it is considered high risk whereas the same for any other race, we consider high risk if it is more than 20 per cent. The bar is set at the lower level for the Indian population.
Clinical practitioners and even lay persons calculate risk score. Easiest risk score they use is by the American Heart Association. This risk score calculator is developed in the form of an app and available on Google as well as Apple store. It is an ASCVD risk calculator. This is an objective app. A person can calculate the risk.
Risk score gives an idea what medication one should take. For example whether a person should take aspirin, cholesterol lowering medication, blood pressure medication, and what lifestyle modification is required. One can also know how much risk reduction is possible by adhering to those lifestyle modifications.
Indians calculating risk on ASCVD need to choose an ‘other’ group which happens to be of South Asian ancestry. More than 20 per cent risk score is considered high risk in the American context while for Indian people, more than 10 per cent risk is considered high risk.
Book Online Consultaion
What Are the 5 Most Common Heart Problems?
Subscribe the Hearty Life Blogs

DR. RAGHU | Best Cardiologist in Hyderabad
Cardiology Coronary, Vascular and
Structural Interventions
A weak heart, also known as heart failure, is a condition characterized by the heart's inability to pump blood efficiently, leading to reduced circulation and inadequate oxygen supply to the body's tissues.
Recent studies have shown that irregular sleep may also increase the risk of cardiovascular problems. In severe cases, it can result in complications, such as heart attacks.
There was a time when people in their 60s, 70s, or 80s had cardiac arrests. But today, a growing number of young people have been succumbing to heart attacks. The tragic part - these people usually...
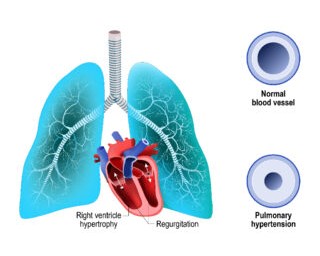
Pulmonary hypertension (PH) is a chronic condition that leads to elevated blood pressure in the pulmonary arteries. It can result in serious complications, including right-sided heart failure, arrhythmias, and even death, if left untreated.
Diagnosing heart failure involves a combination of physical examination, blood tests, and non-invasive procedures like X-rays and ECG.
In our previous articles, we’ve discussed the symptoms of heart failure and the steps to diagnose the same. However, the course of treatment varies for every patient based on the type of heart failure they’ve developed.
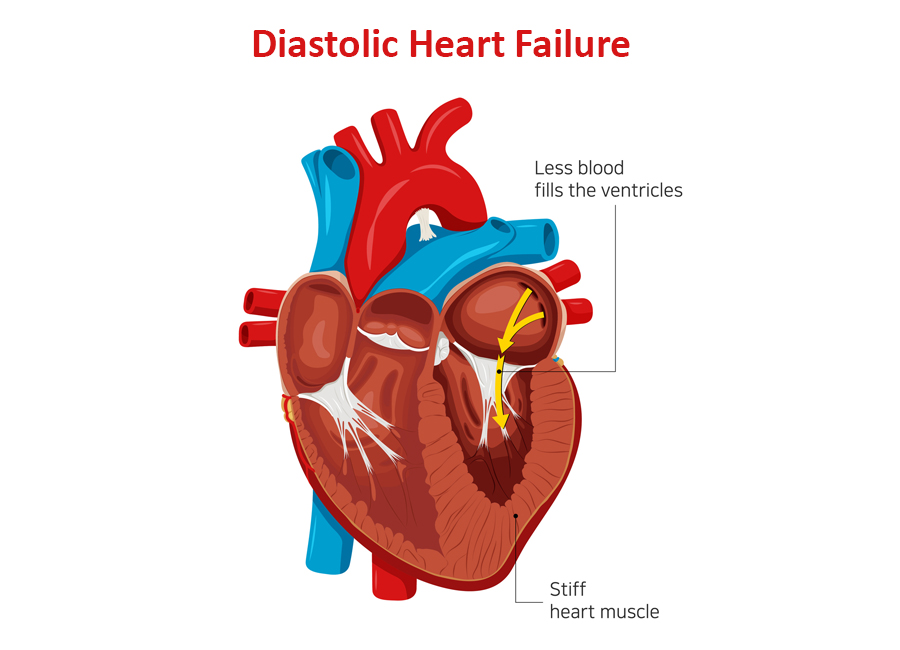
Depending on the part of the heart’s pumping cycle that’s been affected, there are two types of heart failure. In this blog, we’ll take a closer look at diastolic dysfunction and its symptoms.
What Causes Diastolic Dysfunction?
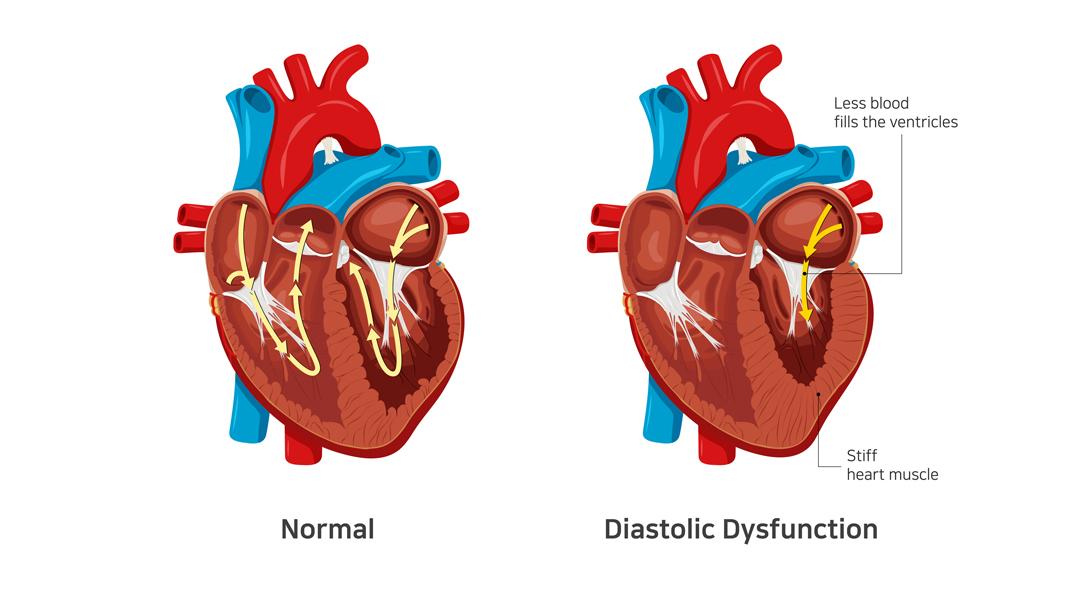
The diastolic phase refers to the part of the heart’s pumping cycle when the ventricles (lower chambers) relax and let blood flow in from the atria (upper chambers). Diastolic dysfunction is a condition in which the ventricles don’t relax enough. That, in turn, prevents the normal amount of blood from entering the heart.
Diastolic dysfunction is caused when the heart muscles become thicker and stiffer than usual. It’s more common in older women with hypertension and diabetes. If left untreated, it can lead to diastolic heart failure (also known as heart failure with preserved ejection fraction).
Related : Understanding Congestive Heart Failure Symptoms
What Does Preserved Ejection Fraction Mean?
Ejection fraction refers to the volume of blood pumped out from the heart’s left ventricle with each contraction. For a healthy heart, the number falls in the range of 55% to 65%. A lower ejection fraction is one of the most common indicators of heart failure.
However, it’s worth noting that many people with diastolic dysfunction have an ejection fraction of 50% or more (which is known as preserved ejection fraction). That means the left ventricle expels an adequate amount of oxygenated blood.
However, the heart muscle doesn’t relax enough to let a sufficient quantity of blood in. That, in turn, causes the excess blood to back up in the lungs and results in fluid buildup in the feet and abdomen.
How to differentiate systolic from diastolic dysfunction ?
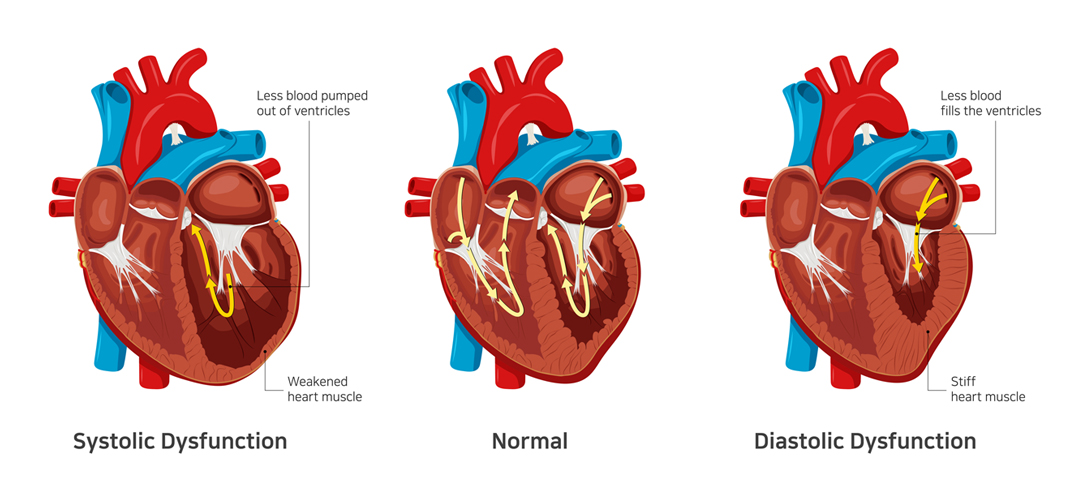
In contrast to systolic dysfunction where the heart muscle is “weak”, in diastolic dysfunction the heart is “stiff”. This means that the heart is unable to pump blood out of the heart in systolic dysfunction whereas the heart is unable to accept further blood in diastolic dysfunction. Both conditions lead to congestion or fluid accumulation in various organs of the body. Differentiation of heart failure from systolic and diastolic dysfunction is not possible as both diseases present with similar symptoms.
Which conditions lead to Diastolic dysfunction?
- Diastolic dysfunction appears consequent to uncontrolled or long-standing diabetes
- Hypertension
- Obesity as well as elderly people
- Women and atrial fibrillation
The best way to prevent and treat diastolic dysfunction is by effective control of the diseases mentioned above.
Symptoms of Diastolic Dysfunction
The most common symptom of diastolic dysfunction is congestion and shortness of breath due to the buildup of blood and fluid in the lungs. Breathing difficulties can get particularly worse during exertion or when lying.
Other symptoms of diastolic dysfunction include:
- Coughing and wheezing (due to lung congestion)
- Loss of appetite and nausea (due to fluid buildup around the liver and in the stomach)
- Swollen feet, legs, and abdomen (due to fluid accumulation)
If you experience any of the given symptoms, it’s crucial to consult a doctor for a proper diagnosis.
Treatment of Diastolic Dysfunction
Treatment of diastolic dysfunction involves a combination of medications (diuretics or water pills) and lifestyle changes. In severe cases, a patient might need left ventricular assist devices or a heart transplant.
Is Diastolic Dysfunction Serious?
In the long run, diastolic dysfunction can lead to diastolic heart failure. That, in turn, increases your risk of hospitalization and death. Therefore, you should pay close attention to your symptoms and reach out to a doctor whenever you notice anything unusual.
Dr. C Raghu is a renowned cardiologist who specializes in interventional cardiology. He has decades of experience in treating patients with different heart conditions. If you or anyone you know has developed symptoms like shortness of breath, swollen feet, loss of appetite, etc., contact Dr. Raghu to explore your treatment options.
Book Online Consultaion
What Are the Symptoms of Diastolic Dysfunction ? – Blog
Subscribe the Hearty Life Blogs

DR. RAGHU | Best Cardiologist in Hyderabad
Cardiology Coronary, Vascular and
Structural Interventions
Conditions & Diseases

Angioplasty

Aortic Stenosis

Atrial Fibrillation