Inferior vena cava (IVC) is the large vein in your abdomen that carries deoxygenated blood from the lower part of the body back to the heart. This vein branches out throughout the body to transport deoxygenated blood to the heart

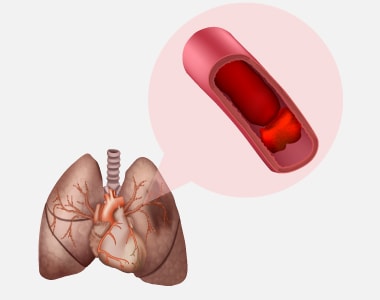
Deep vein thrombosis (DVT) is a serious medical condition where blood clots are formed in the deep vein of the thigh or lower leg. This causes pain, swelling, and tenderness in the leg. The clot formed can break free, travel to the lung and stick to a vessel in the lung. This can lead to a blockage in the vessel, called pulmonary embolism, which can cause severe shortness of breath and sudden death. An IVC filter placement is one option to prevent pulmonary embolism.
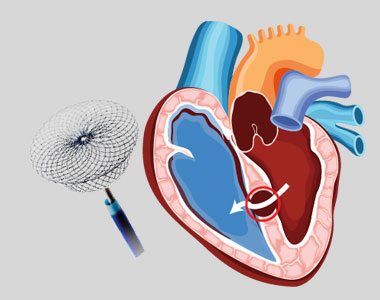
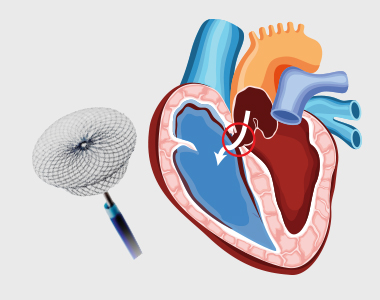
Inferior vena cava (IVC) filter placement involves insertion of a filter into the IVC through a small incision made in the neck or groin. An IVC filter is a small, metal device shaped like the spokes of an umbrella. When the filter is placed in the IVC, the filter catches the blood clots and prevent them from reaching the lungs.
Indications for IVC filter placement
IVC filter placement is considered when anticoagulants (blood thinners) cannot be used to prevent the formation of blood clots.
The following conditions are indicative of IVC filter placement:
- You have or had DVT or pulmonary embolism
- Anticoagulants-associated bleeding
- Severe platelet problems or shortages
- Recurrence of blood clots while on anticoagulants
- Recent or current major bleeding that cannot be treated
- Bleeding in your head
- A need for surgery in the near future
- Multiple broken bones
The risks of IVC filter placement procedure:
IVC filter placement is usually a safe procedure. Sometimes, the following problems may occur during the procedure:
- Filter blocks the inferior vena cava, leading to swelling of the leg
- Failure of the filter sooner or later
- Filter moves or travels to the heart or lungs
- Damage to the vein (rare) or other structures/organs
- Bleeding
- Infection
- Allergic reactions to medicines or dyes
- A pool of blood (hematoma) around the site where a flexible tube is inserted (catheter insertion site).
What happens before the procedure?
When planning for the procedure, inform your doctor about:
- Any blood disorders or other medical conditions you have.
- The medicines or supplements you are taking, such as over-the-counter drugs, vitamins, herbs, creams, or eye drops.
- Any allergies, including iodine allergy.
- Problems associated with anaesthetic medicines you or family members have or had.
- The surgeries you have undergone.
- If you are or may be pregnant.
Preparations for the procedure:
1. Staying hydrated:
Your healthcare provider may instruct about hydration before the procedure:
- Up to 2 hours before the procedure- you may drink clear liquids, such as water, clear fruit juice, black coffee, and plain tea.
2. Eating and drinking restrictions:
Your healthcare provider may give some guidelines related to eating and drinking, such as:
- 8 hours before the procedure – stop eating heavy meals or foods such as meat, fried foods, or fatty foods.
- 6 hours before the procedure – stop eating light meals or foods, such as toast or cereal.
- 6 hours before the procedure – stop drinking milk or drinks that contain milk.
- 2 hours before the procedure – stop drinking clear liquids.
3. Medicines:
Ask your health care provider about:
- Changing or stopping your regular medicines, especially diabetes medicines or blood thinners.
- Taking medicines such as aspirin and ibuprofen, as these can thin your blood. Do not take these medicines before your procedure if your health care provider instructs you not to.
- Taking any antibiotic medicine to help prevent infection.
General instructions:
- Ask your health care provider how your surgical site will be marked or identified.
- You may have blood tests to tell how well your kidneys and liver are working. They can also show how fast your blood is clotting.
- You may be asked to shower with a germ-killing soap.
- Ensure that you have someone take you home from the hospital or clinic.
- If you will be going home right after the procedure, plan to have someone with you for 24 hours.
- Do not use any products containing nicotine or tobacco, such as cigarettes and e-cigarettes. If you need help quitting, ask your health care provider.
What happens during the procedure?
Before heading to the procedure, to lower the risk of infection, your healthcare team will:
- Wash or sanitize their hands
- Wash your skin with soap
- Remove hair from the surgical area
- Insert an IV tube into one of your veins
You will be given one or more of the following:
- A medicine to help you relax (sedative)
- A medicine to numb the area (local anaesthetic)
Once the anaesthesia sets in, the steps below may be followed:
- A small cut (incision) will be given in the neck or groin region to access the IVC.
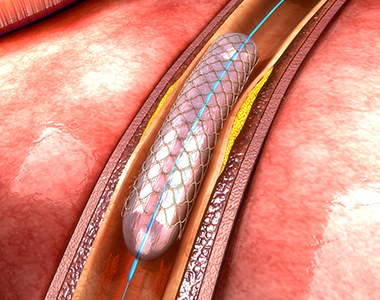
- A flexible tube (catheter) will be inserted in the incision.
- Contrast dye may be injected into the IVC to help guide the catheter reach the precise vein.
- X-rays may be used to make sure that the catheter is in the correct position.
- The filter will be inserted into the vein through the catheter and it will be positioned at the correct location in the IVC.
- The catheter will be removed.
- Pressure will be applied to the insertion site to stop bleeding.
- A bandage (dressing) may be applied over the catheter insertion site.
- Your IV tube will be taken out.
The procedure may vary among health care providers and hospitals.
What happens after the procedure?
Your blood pressure, heart rate, breathing rate, and blood oxygen level will be monitored until the medicines you were given have worn off.
Your insertion site will be monitored for the first few hours for any signs of bleeding.
Do not drive for 24 hours if you were given a sedative.
Call your provider immediately if you have:
- Numbness or coldness in one of your limbs
- Bleeding that won’t stop with pressure
- Severe pain or swelling at the incision site
- Fluid leakage from the incision site
- Redness or warmth at the incision site
- Fever
- Severe headache or nausea
- Chest pain