Aortic valve stenosis is a serious condition that doesn’t just affect the aortic valve. It reduces or blocks the blood supply to the aorta. That, in turn, restricts blood flow to vital organs, including the brain, kidneys, and liver.
Resources | Dr Raghu - Page 2
Grading Severity of Aortic Stenosis
Aortic valve stenosis is a serious disease that can lead to heart failure, strokes, and even death if left untreated. That makes timely diagnosis and treatment of the condition crucial. However, treatment of aortic stenosis depends on its severity.
Typically, the following parameters are used to determine the severity of aortic stenosis:
- Pressure gradient – High gradient (HG; >/=40 mm Hg) or low gradient (LG; <40 mm Hg)
- Blood flow – Normal flow (NF; SVi>35 ml/m2) or low flow (LF; SVi<35ml/m2)
- Left ventricular ejection fraction (LVEF) – Preserved (>/=50%) or reduced (<50%)
Depending on the pressure gradient and blood flow parameters, aortic stenosis is graded as follows:
- Normal flow-low gradient (NF-LG)
- Normal flow-high gradient (NF-HG)
- Low flow-high gradient (LF-HG)
- Low flow-low gradient (LF-LG)
NF-HG is the most prevalent type of aortic stenosis and has well-established management protocols. Patients with NF-HG are also ideal candidates for aortic valve replacement. While LF-LG is fairly rare, it’s often associated with a poor prognosis.
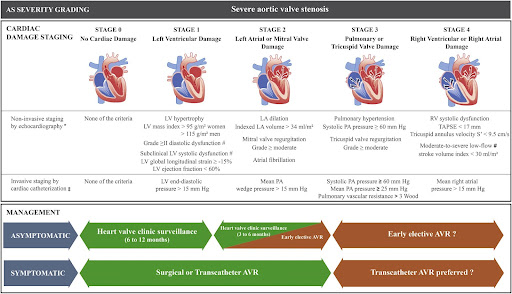
Additionally, depending on progression, heart valve disease can be categorized into the following four stages:
- Stage A (At risk) – Characterised by the presence of risk factors
- Stage B (Progressive) – Mild or moderate valve disease with no noticeable symptoms
- Stage C (Asymptomatic severe) – Severe valve damage with no noticeable symptoms
- Stage D (Symptomatic severe) – Severe valve disease with noticeable symptoms
Doctors use a variety of diagnostic tests to evaluate the aforementioned parameters and determine the severity of aortic stenosis. If you experience symptoms like chest pain, heart murmur, or palpitation, it’s crucial to reach out to an experienced cardiologist and get the right treatment for aortic valve stenosis.
How Does One Diagnose Aortic Stenosis – ECG, ECHO, TEE, or CT aortogram?
Early diagnosis of aortic valve stenosis is crucial to prevent severe complications, such as arrhythmias, heart failure, stroke, and death. Also, it can help administer timely treatment, thus improving the patient’s prognosis and quality of life.
That’s why cardiologists use a series of tests to diagnose aortic valve stenosis and its underlying cause. When you visit the doctor, they’ll start by asking you about your symptoms and medical history. Also, they ask whether your family has a history of cardiovascular ailments. Next, they’ll use a stethoscope to detect the presence of the characteristic aortic stenosis murmur.
Additionally, your doctor will use one or more of the following tests for the complete diagnosis:
- ECG (Electrocardiogram) – It’s one of the most preliminary tests that evaluate the heart’s electrical activity and helps doctors identify an irregular heartbeat and other abnormalities.
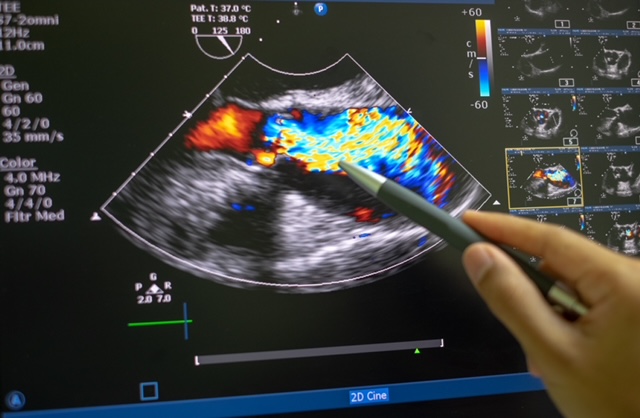
- Echo (Echocardiogram) – It uses sound waves to generate images of the beating heart. It helps doctors examine how blood flows through each valve and determine the severity of aortic stenosis.
- TEE (Transesophageal echocardiogram) – It’s a special type of echocardiogram in which an ultrasound probe is inserted into the esophagus and directed closer to the heart. It helps doctors take a closer look at the aortic valve and identify the underlying cause of aortic stenosis.
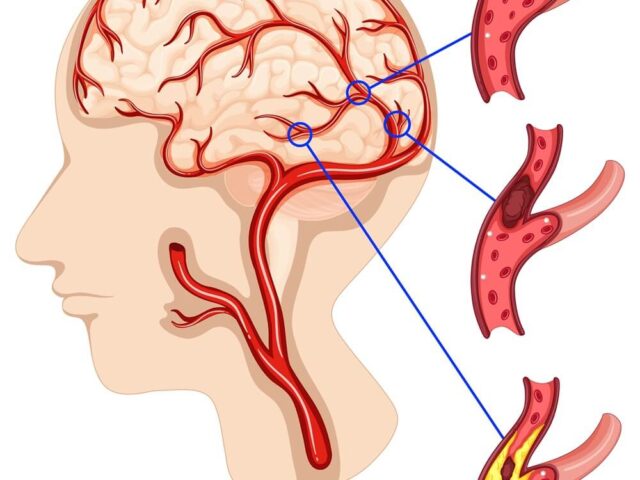
- CT aortogram – It’s used to evaluate the blood supply to the upper body and identify conditions such as atherosclerosis.
Additionally, your doctor might recommend tests like cardiac catheterization and chest X-ray to get a complete picture of your cardiac health and plan the right course of treatment.
Book Online Consultaion
Diagnosing Aortic Stenosis – Blog
Subscribe the Hearty Life Blogs
Basics of the Heart
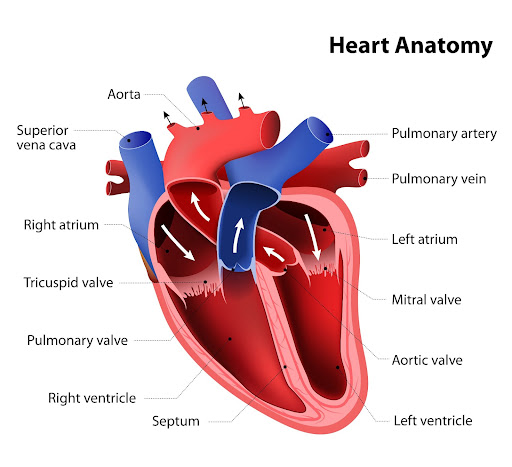
The heart is a vital organ of the human body. It pumps blood throughout your body and keeps you alive. It comprises cardiac muscle tissue. That means the heart can contract and relax to squeeze blood out of the heart and into your body. It supplies blood to all organs, including the brain, kidneys, liver, and more.
The heart has four chambers divided by two walls called septa. The upper chambers are called the atria, and the lower chambers are called the ventricles.
The atria receive blood from the veins and pump it into the ventricles through openings called valves. The tricuspid valve separates the right atrium from the right ventricle, and the mitral valve separates the left atrium from the left ventricle. There’s also a pulmonary valve that sits between the right ventricle and the pulmonary artery.
Then there’s the aortic valve located between the left ventricle and the aorta. It prevents blood from leaking back into the left ventricle during the contraction phase of the heart’s pumping cycle.
When your heart beats, it squeezes blood out through an opening in each chamber called an aortic valve into either a large artery (aorta) or one of its branches, the carotid arteries, before heading back down to smaller arteries throughout your body. When the heart pumps blood to other organs, oxygen will be picked up by red blood cells as they pass through capillaries.
What Is the Aortic Valve, and Why Is It Important?
The aortic valve is one of the four valves in the heart. It is a flap of tissue that keeps blood flowing in one direction. It is located in the middle of the heart, between the left ventricle and the aorta, the main artery that supplies blood throughout the body. The aortic valve is a semilunar valve, meaning the flaps of the valve are crescent-shaped.
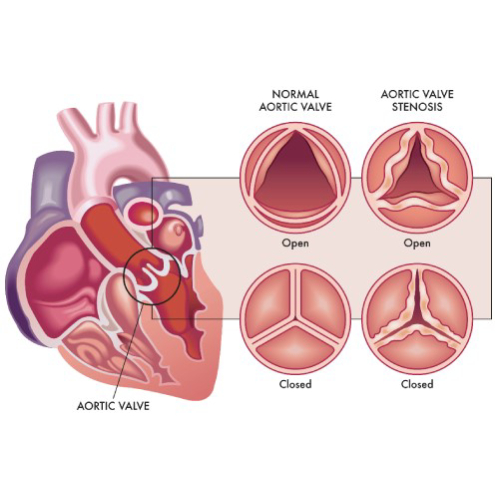
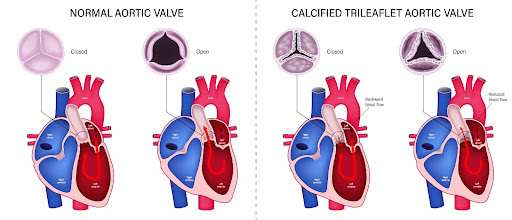
The aortic valve comprises three sections called leaflets or cusps. Each cusp is made of collagen. Some people are born with only two cusps in the aortic valve. In such cases, it is known as a bicuspid aortic valve.
The aortic valve opens when the heart contracts or squeezes and closes when the heart relaxes. It lets oxygen-rich blood flow from the left ventricle into the aorta for circulation throughout your body.
The aortic valve is crucial because it ensures that blood keeps flowing in the right direction from the heart. It prevents the backflow of blood from the aorta into your left ventricle.
If the aortic valve doesn’t work properly, it can cause serious problems. A leaky or stiffened valve won’t open and close properly, which means that some blood flows backward into the left ventricle. It puts extra pressure on the heart and can lead to heart failure or stroke if severe enough.
Which Diseases Affect the Aortic Valve?
The aortic valve is a crucial part of the heart that keeps blood flowing in the right direction throughout the body. The two primary diseases that affect the aortic valve are:
- Aortic valve stenosis
- Aortic valve regurgitation
In aortic valve stenosis the cusps (or flaps) of the aortic valve become stiff and thick, thus narrowing the valve opening. That, in turn, restricts blood flow from the heart’s left ventricle to the aorta and the rest of the body.
Aortic valve stenosis is usually caused by pre-existing conditions, such as congenital heart defects, aortic valve calcification, and rheumatic fever. Chronic ailments, such as hypertension, endocarditis, and diabetes, and treatments like radiation therapy to the chest can also increase the risk of aortic valve stenosis.
In aortic valve regurgitation, the flaps don’t close properly, causing a backflow of blood into the left ventricle. As with aortic valve stenosis, this condition is also caused by pre-existing ailments that affect the heart.
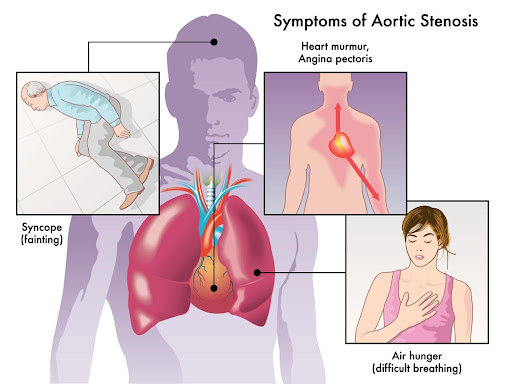
Common symptoms of aortic valve disease include heart murmur, chest pain, dizziness, fatigue, irregular heartbeat, and shortness of breath. Treatment for these conditions depends on the severity of the disease and its underlying cause. If left untreated, both aortic valve stenosis and aortic valve regurgitation can lead to heart failure and other complications.
| According to the CDC, nearly 2.5% of the US population suffers from heart valve diseases. These conditions are more common in older people, with 13% of people born before 1943 experiencing them. Also, 1% to 2% of the US population is affected by the bicuspid aortic valve, with the condition being more common in men. |
If you experience any of the aforementioned symptoms, reach out to an experienced cardiologist for proper diagnosis and treatment.
Aortic Stenosis: What Is It?
Aortic stenosis is a heart valve disease affecting the aortic valve that connects the heart’s left ventricle (lower chamber) to the aorta (main artery). The aortic valve is responsible for ensuring that blood flows in one direction throughout the body.
In aortic valve stenosis, the aortic valve flaps (or cusps) become stiff or thick due to calcium buildup in the valve or other underlying causes. It causes the valve opening to become narrow and restricts blood flow to the aorta. That, in turn, reduces or blocks the blood supply to vital organs, such as the liver, kidney, brain, etc.
Symptoms of aortic valve stenosis include:
- A whooshing or swishing heart sound (known as aortic stenosis murmur)
- Chest pain or tightness
- Fatigue and dizziness (particularly after physical activity)
- Shortness of breath
- Palpitations
Depending on the underlying cause, there are two types of aortic stenosis – congenital and acquired. Congenital aortic stenosis is present from birth due to a defect in the valve’s formation. Acquired stenosis develops after birth due to other heart-related ailments, such as hypertension, endocarditis, rheumatic fever, and aortic valve calcification.
The risk of aortic stenosis increases in older people. Also, people who have received radiation therapy to the chest are more vulnerable to the condition.
Treatment for aortic valve stenosis depends on the underlying cause and the severity of the condition. Many patients need surgery to repair the valve. If left untreated, aortic stenosis can lead to heart failure, stroke, arrhythmias, and even death. Therefore, it’s crucial to diagnose aortic valve stenosis and treat the condition at the earliest.
Book Online Consultaion
Understanding Aortic Stenosis – Blog
Subscribe the Hearty Life Blogs
Regular consumption of artificial sweeteners like aspartame and sucralose can have an adverse effect on your heart. They increase your risk of coronary heart disease, strokes, and other ailments.
Aspirin is one of the most widely used over-the-counter drugs in the world. It comes in several forms, but the most common way to take it is as a pill. It belongs to a specific class of medications called nonsteroidal anti-inflammatory drugs (NSAIDs).
Many people have heart disease, but not all of them know it. Doctors use a variety of tests to identify cardiac ailments and their underlying causes. Coronary angiography is one of the most common diagnostic tests that doctors use.
While it’s considered a safe and minimally invasive procedure, coronary angiography comes with a few risks. You can read more about the potential risks and complications in our previous blog.
The good news is that you can avoid side effects with proper care after the procedure. If you’ve recently had coronary angiography or are going through one soon, here is what you need to do after the procedure:
Avoid Heavy Physical Activity
It’s important to rest after coronary angiography. Avoid lifting heavy objects or resuming your exercise routine right after the procedure. Make sure you get plenty of sleep and let your body and mind relax for at least a week after angiography. Ask your doctor if you’re unsure when to hit the gym or start exercising.

Embrace Healthy Habits
Avoid cigarettes for at least a few days if you are a smoker. Smoking can cause spasms in the coronary arteries, leading to a heart attack or stroke after your angiography. Also, avoid alcohol consumption, and make sure you eat a balanced diet.
If you are a coffee drinker or have high blood pressure, avoiding all caffeine products (coffee, tea) and salt for several days following your procedure may be a good idea. The most important thing is to listen carefully to what your doctor tells you about caring after coronary angiography to avoid any other complications during recovery or later down the road.
Be Careful About Removing the Bandage
A crucial step to caring after coronary angiography is to avoid removing the bandage until the morning of the second day after the procedure. Also, you should not remove it yourself. Let someone else help you remove it. You must consult your doctor or nurse before removing the bandage.
Expect Soreness and Pain for a Few Days
Your arm or leg (where the catheter was inserted) might feel sore for a few days following a coronary angiogram. The discomfort you feel is usually caused by the catheter or dye used for the test.
The catheter may have been left in place too long, leading to irritation and inflammation. Or it could be a reaction to the dye that was used to take images of your arteries during the procedure. It can also happen if you’re allergic to any component of either one.
In most cases, the pain and soreness should subside after a few days. If the pain persists or the arm/leg becomes numb, it’s a good idea to reach out to your doctor. Also, if you have a fever or trouble breathing, call your doctor right away.
If you are bleeding from the incision site, apply direct pressure with a gauze dressing until the bleeding stops. Don’t remove the dressing unless instructed by medical staff at the hospital.
Conclusion
Coronary angiography is a safe and effective procedure that can give you a better understanding of your heart health. If you follow your doctor’s instructions, you’ll be on the road to recovery in no time.
Dr. C Raghu is a renowned cardiologist who has treated thousands of patients with cardiac ailments. If you have any concerns or questions about coronary angiography, feel free to reach out to Dr. Raghu today.
Book Online Consultaion
Care After Coronary Angiography – Blog
Subscribe the Hearty Life Blogs

DR. RAGHU
Cardiology Coronary, Vascular and
Structural Interventions
Conditions & Diseases

Angioplasty

Aortic Stenosis

Atrial Fibrillation

Atrial Septal Defect
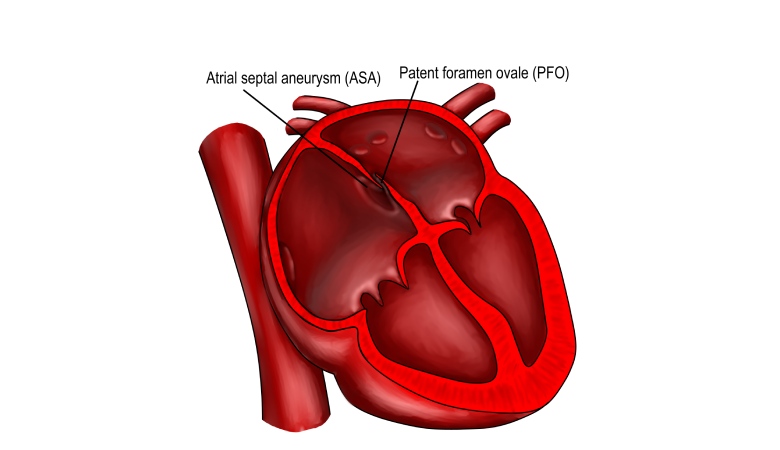
Patent Foramen Ovale (PFO) is a hole in the heart that can be congenital or acquired. The foramen ovale is a flap-like opening between the heart’s upper chambers. It usually closes within three to six months after birth and becomes a part of your heart’s septum.
Cardiac catheterization is a procedure that uses a thin tube (called a catheter) to examine the heart and blood vessels. The catheter is inserted into a blood vessel in the groin or arm.
Doctors use various diagnostic tests to assess cardiac health and diagnose conditions like coronary artery disease and heart failure. While a coronary angiogram is commonly used to identify these conditions, your doctor can prescribe other tests like CT coronary angiography.
In our previous blogs, you can read more about the use cases and risks of coronary angiography. In this article, we’ll delve deeper into CT coronary angiography and understand why it’s crucial for people with cardiac ailments.
What Is CT Coronary Angiography?
CT coronary angiography is a type of CT scan that uses special dyes to evaluate the heart’s blood vessels. It can detect blockages in the coronary arteries that supply blood to the heart. It can identify blockages that are too small for other methods, such as a regular angiogram or an electrocardiogram (ECG), to pick up.

A CT coronary angiography scan aims to find any abnormal areas in your coronary arteries that could be causing stenosis (narrowing) or occlusion (blockage). It helps doctors identify underlying heart-related ailments and determine the right course of treatment.
How Does CT Coronary Angiography Work?
The test is usually done in a hospital or clinic. To begin with, the doctor or radiologist will start an intravenous (IV) line to administer the contrast dye. As the contrast flows through your veins, it will appear on the scan as bright white areas on a black background. It’ll help the doctor see your heart and coronary arteries.
The test usually lasts about 30 minutes to one hour. The CT coronary angiogram procedure involves two scans: one with diastolic blood flow and another with systolic blood flow.
When Is CT Coronary Angiography Used?
CT coronary angiography is used to diagnose a heart attack and evaluate blood flow in the heart. Also, doctors use it to detect blockages in arteries that supply blood to the heart muscle.
What Are the Risks of CT Coronary Angiography?
While CT coronary angiography is a non-invasive and safe procedure, it can cause the following side effects:
- You may have an allergic reaction to the contrast dye.
- Your body will be exposed to high levels of radiation, which can increase your risk of developing cancer.
- You might have to pay out of pocket because the test isn’t always covered by insurance.
- You might experience more anxiety and stress if the scans indicate blockages in your arteries.
What Should I Expect When Having CT Coronary Angiography?
If you are planning to get a CT coronary angiography, you should be prepared for the following:
- The radiologist will ask you to change into a hospital gown.
- The radiologist will give you an injection of a contrast dye.
- You will lie on a table, and the table will move into the CT scanner.
- The scan is painless and takes about 20 minutes.
Conclusion
CT coronary angiography is a painless and safe test that can help determine if you have blocked arteries. If you have chest pain, you should consider getting the test done as soon as possible because it may save your life.
Dr. C Raghu is a renowned cardiologist with decades of experience. He specializes in interventional cardiology and has treated thousands of patients with cardiac ailments. If you or anyone you know is experiencing symptoms like chest pain, breathlessness, palpitations, etc., reach out to Dr. Raghu today.

DR. RAGHU | CT Coronary Angiography in Hyderabad
Cardiology Coronary, Vascular and
Structural Interventions
Conditions & Diseases

Angioplasty

Aortic Stenosis

Atrial Fibrillation

Atrial Septal Defect
Coronary angiography is a procedure that uses X-rays to visualize and inspect arteries. It shows if there are any blocked arteries and how well your heart muscle is working.