The most likely cause of right sided heart failure is a weak left ventricle. In other words, left sided heart failure eventually leads to right sided heart failure.
Resources | Dr Raghu - Page 4
Depending on the side of the heart that’s been affected, heart failure can be of two types – left-sided and right-sided. We’ve already discussed the causes and symptoms of right sided heart failure in one of our previous blogs.
It’s now time for us to dig deeper into left sided heart failure, which is the most likely cause of right sided heart failure. Let’s jump right in.
Related: What Is a Normal Ejection Fraction by Age?
What Is Left Sided Heart Failure?
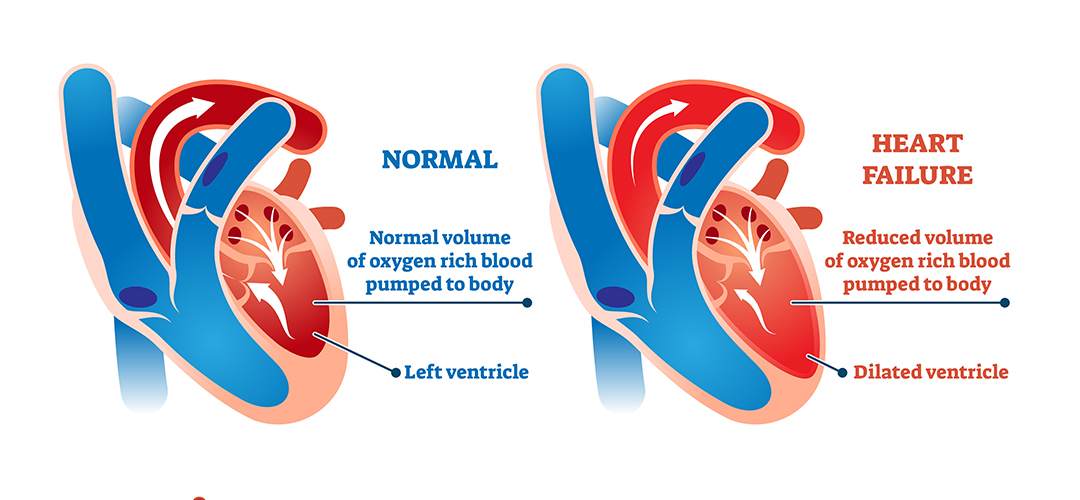
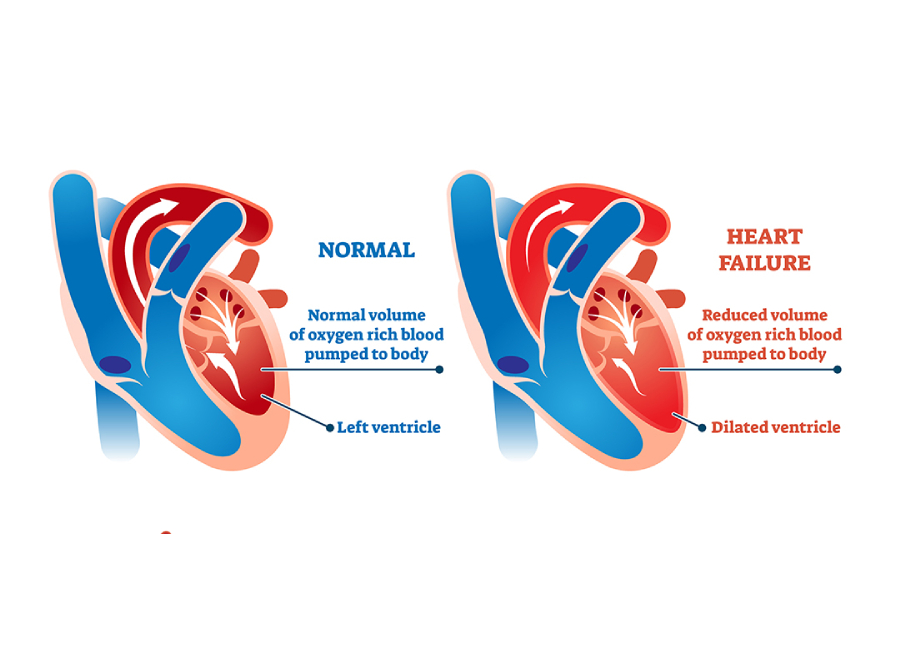
Left sided heart failure is characterized by a decline in the heart’s pumping function. In this condition, the heart gradually loses its ability to pump blood from the left ventricle into the arteries.
The ejection fraction for a patient with left sided heart failure is often lower than 50%. That, in turn, leads to a buildup of blood in the lungs and fluid in the body. Also, left sided heart failure depletes vital organs of oxygen-rich blood.
Related: What Is Systolic Heart Failure?
What Are the Symptoms of Left Sided Heart Failure?
The most common left sided heart failure symptoms include:
- Shortness of breath
- Coughing and wheezing
- Weight gain (due to fluid buildup)
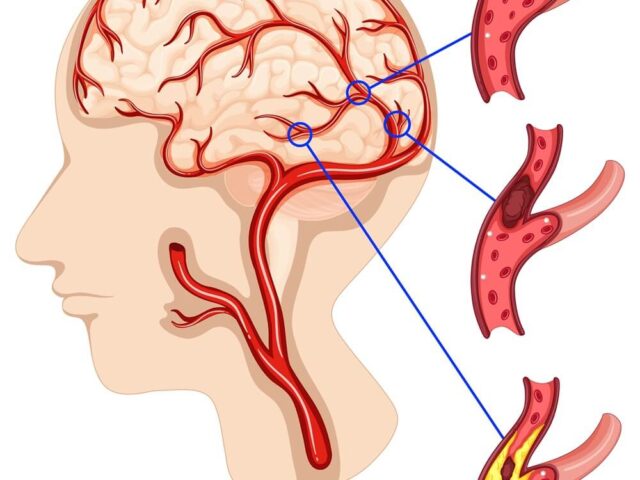
Additionally, a lack of an adequate blood supply to the brain can cause confusion. Also, it can result in fatigue.
What Causes Left Sided Heart Failure?
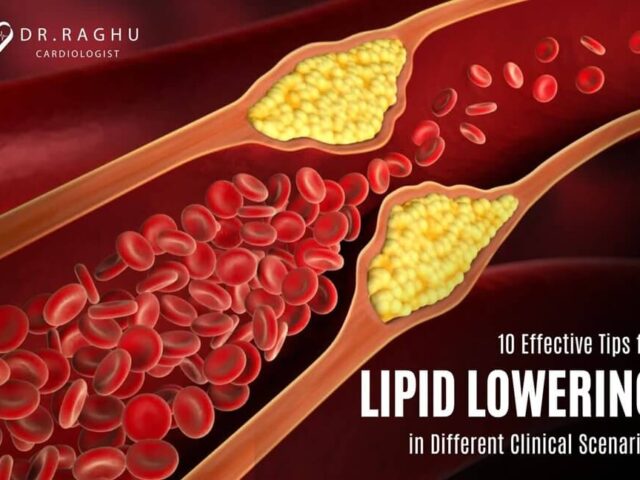
Left sided heart failure is the result of a gradual weakening of the heart’s left ventricle. It can happen due to underlying conditions, such as coronary artery disease, hypertension, and heart valve damage. It can also be the result of heart muscle damage due to a previous heart attack.
Related: Understanding Congestive Heart Failure Symptoms
Treatment of Left Sided Heart Failure
Doctors treat left sided heart failure based on its underlying cause. They can prescribe medication, such as ACE inhibitors and beta-blockers, to manage conditions like hypertension. Additionally, many patients are prescribed diuretic pills to prevent fluid buildup due to heart failure.
Left sided heart failure treatment also involves a healthy diet and lifestyle changes. For instance, a doctor might recommend that you follow an exercise routine and lose weight. Also, they’ll ask you to avoid smoking and alcohol consumption.
Left Sided Heart Failure vs. Right Sided Heart Failure
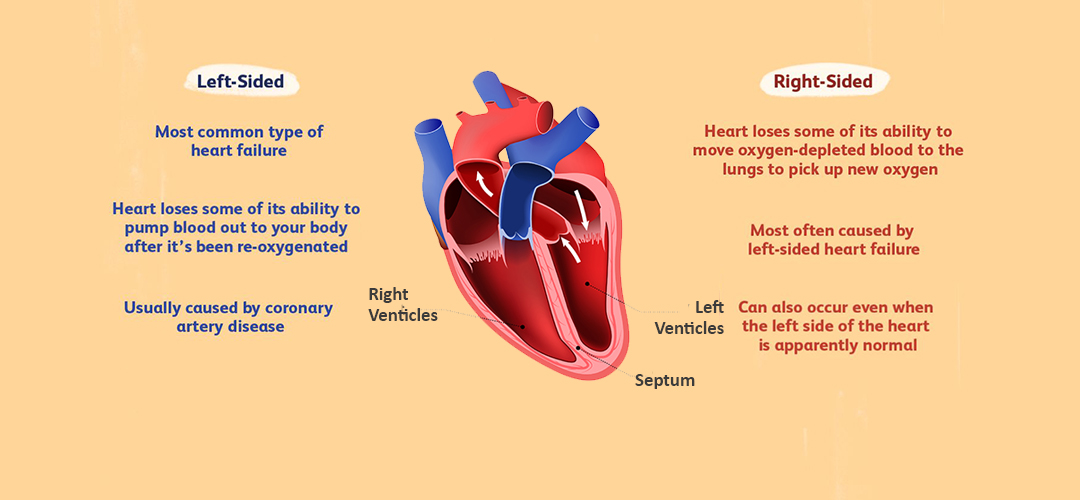
In right sided heart failure, the right ventricle becomes weak and has trouble pumping deoxygenated blood to the lungs. It’s usually a result of progression of a left sided heart failure. People with right heart failure present with swelling of feet, face, abdomen and distended pulsatile neck veins. They can also present with generalised weakness and easy fatiguability.
When the left ventricle doesn’t pump out an adequate amount of oxygenated blood to the circulatory system, some of the excess blood flows back into the lungs. This leads to breathlessness as the predominant symptom of left heart failure. This breathlessness can present initially on unaccustomed exertion to progress with less severe exercise and finally to breathlessness on lying flat. Left heart failure in turn, makes it difficult for the right ventricle to pump deoxygenated blood to the lungs. In the long run, it exerts the walls of the right ventricle and results in right sided heart failure.
In Conclusion
Left sided heart failure is a serious condition that can result in organ damage and right sided heart failure. The condition can be treated with a combination of medicines, like beta-blockers and diuretics, and lifestyle changes.
Dr. C Raghu is an eminent cardiologist with more than two decades of experience. He’s been treating patients with various heart conditions, helping them live longer and healthier lives. If you or anyone you know has developed symptoms of left sided heart failure, don’t hesitate to consult Dr. Raghu right away.

DR. RAGHU | Best Cardiologist in Hyderabad
Cardiology Coronary, Vascular and
Structural Interventions
Conditions & Diseases

Angioplasty

Aortic Stenosis

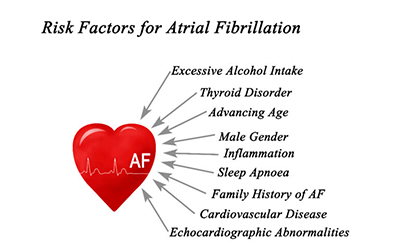
Atrial Fibrillation

Atrial Septal Defect
The heart is a critical organ that powers the human body. It beats roughly 100,000 times a day and pumps more than 2,000 tons of blood throughout the body.
Heart failure is a condition in which the heart gradually loses its pumping capacity. It can lead to symptoms like breathlessness, fluid buildup, and mental confusion. In the long run, it can result in organ damage and even death.
In this blog, we’ll take a closer look at the symptoms, causes, and treatment of congestive cardiac failure. Let’s dive right in.
Congestive Cardiac Failure and Heart Failure: Are They the Same?
Traditionally, doctors used the terms congestive cardiac failure or congestive heart failure to refer to the progressive deterioration of the heart’s pumping action. They used “congestion” to describe the buildup of fluid in the lungs due to heart failure.

However, subsequent studies have shown that the condition can lead to other symptoms, such as swollen feet, fatigue, and mental confusion. That’s why doctors use the term heart failure nowadays.
Causes of Congestive Heart Failure
Irrespective of whether you call it congestive cardiac failure or simply heart failure, its most common causes include:
- Heart valve damage
- Diabetes
- Heart rhythm disturbances
Additionally, damaged or dying heart tissue due to an infection or a previous heart attack can result in congestive cardiac failure.
Related : Mitral Valve Stenosis : Symptoms, Diagnosis, Treatment
Symptoms of Congestive Heart Failure
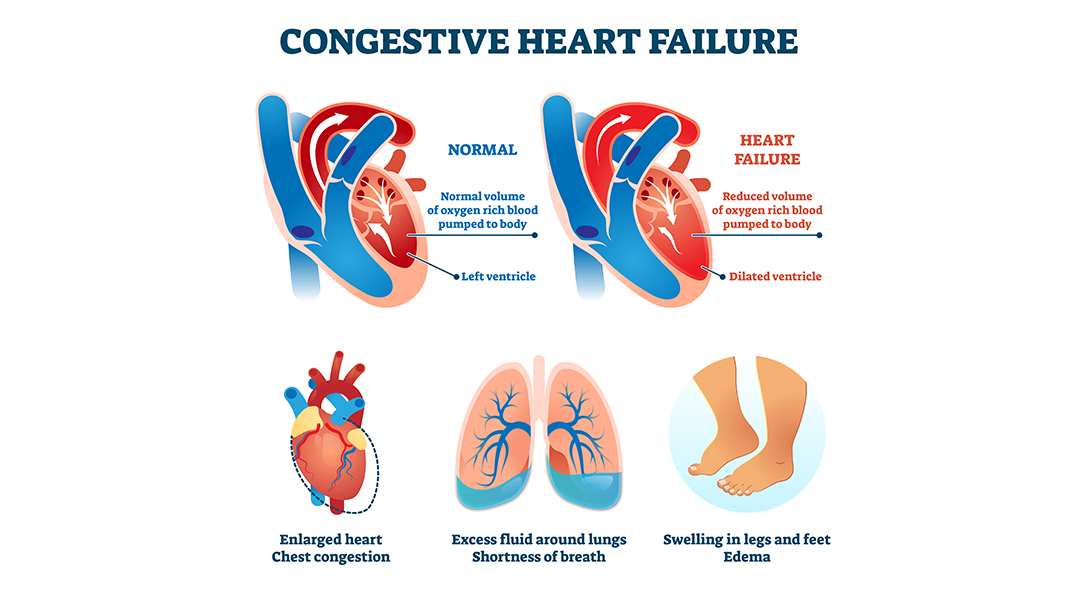
The symptoms of congestive heart failure depend on whether it causes a lack of oxygen supply to the organs or excess fluid buildup in the body.
In the first case, the symptoms include mental confusion, fatigue, and discolored or bluish skin. In the second case, heart failure can lead to symptoms, such as shortness of breath, coughing, wheezing, weight gain, swelling in the feet, legs, and abdomen, and loss of appetite.
Treatment of Congestive Heart Failure
The treatment of congestive heart failure depends on its underlying cause and the side of the heart that’s affected. A doctor will order a series of tests, such as chest X-ray, ECG, echocardiogram, and coronary angiography. Routine blood tests, such as lipid panel and electrolyte tests, might be needed, too.
Once the root cause is identified, your doctor can prescribe one or more of the following medications:
- Diuretic or water pills
- Beta-blockers
- ACE inhibitors or Angiotension receptor Neprilysin inhibitor
- Digoxin
- Anticoagulants
Additionally, the doctor will recommend lifestyle changes, including exercise, a low-sodium diet, and weight loss. Also, they’ll ask you to quit smoking and limit alcohol consumption. In extreme cases, patients need a heart transplant or ventricular assist device (VAD) to improve their quality of life.
Wrapping Up
Congestive cardiac failure is a chronic condition with no known cure. If left untreated, it can lead to organ damage and death. However, a proper treatment plan comprising lifestyle changes and medications can help manage various symptoms.
Dr. C Raghu is a renowned cardiologist and a specialist in interventional cardiology. If you or anyone you know is experiencing symptoms of heart failure, don’t hesitate to contact Dr. Raghu right away.
Book Online Consultaion
Congestive Cardiac Failure – Blog
Subscribe the Hearty Life Blogs

DR. RAGHU | Best Cardiologist in Hyderabad
Cardiology Coronary, Vascular and
Structural Interventions
Conditions & Diseases

Angioplasty

Aortic Stenosis

Atrial Fibrillation

Atrial Septal Defect
Atrial fibrillation is a progressive heart disease that can’t be cured. But the right course of treatment can help control afib symptoms and help patients live a close-to-normal life.
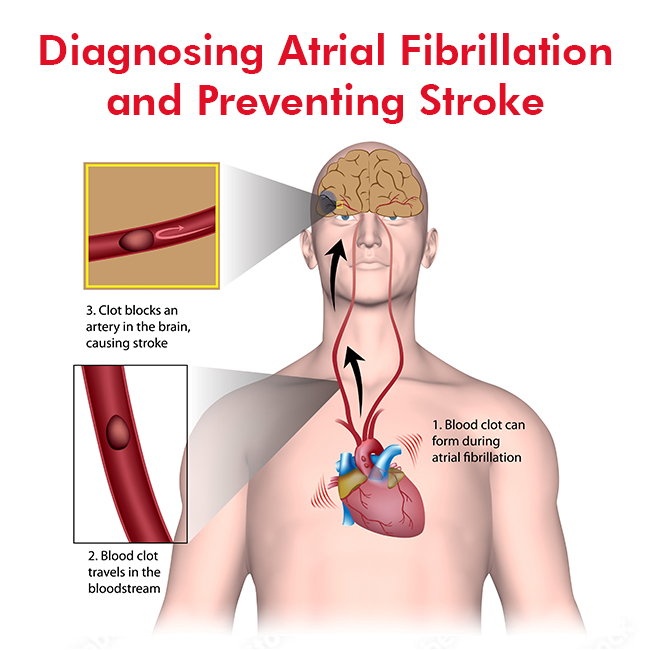
Atrial fibrillation (AFib) interferes with the normal functioning of the heart. It can lead to blood clots, which, in turn, can result in a stroke or heart failure. That makes it crucial to diagnose the condition early on and start the necessary treatment.
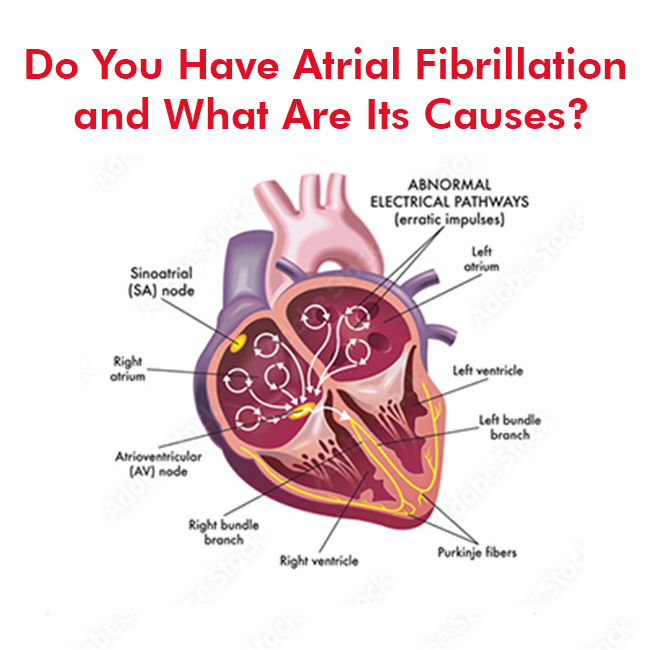
Atrial fibrillation, also known as afib or A-fib, is a medical condition that causes the heart to beat irregularly and quickly. It affects more than 3 million people in the US.
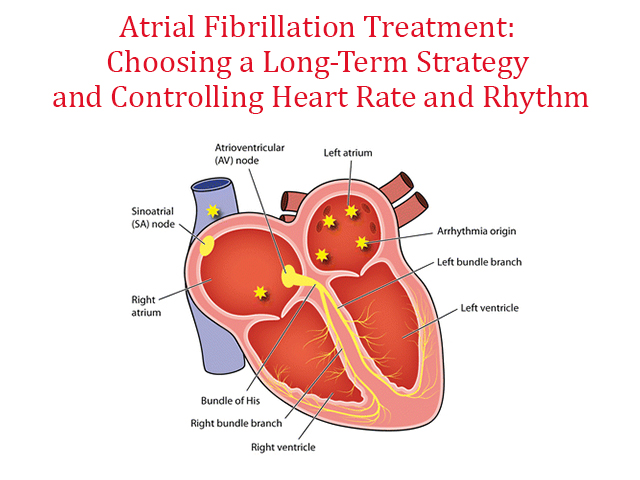
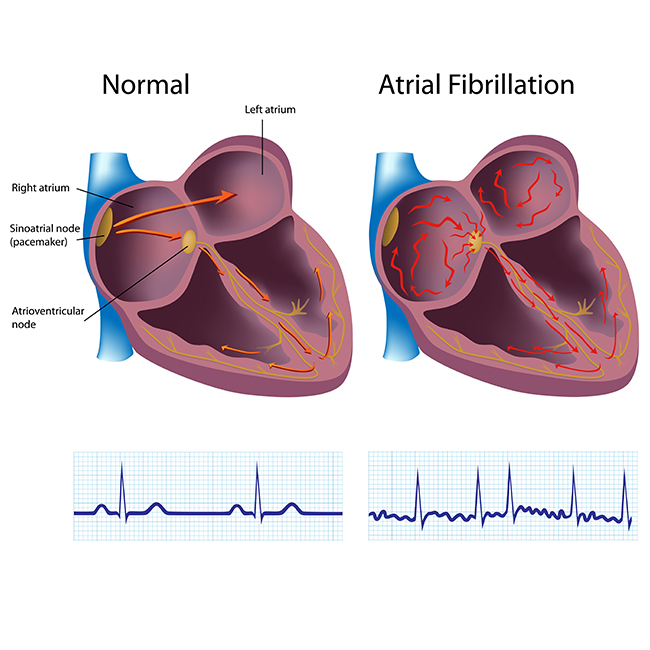
Atrial fibrillation (AFib or AF) is when your heart’s upper chambers (Atria) beat irregularly and out of sync. The heart’s pumping function isn’t as strong or efficient as it should be because the atria aren’t squeezing in rhythm as they should be.
Atrial fibrillation (AFib) is one of the most common heart arrhythmias (irregular or abnormal beating). It happens when your heart’s upper chambers (the atria) beat abnormally fast and out of rhythm.
ECG is a simple inexpensive test to asses heart function. ECG is the short form for electrocardiogram or electrocardiography.
Heart failure can be categorized into different types depending on various factors. While most conditions cause similar symptoms, clear identification of the type of heart failure is crucial for doctors to determine the proper course of treatment.