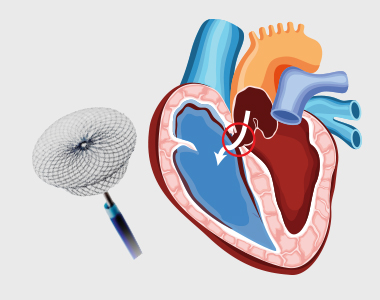
An atrial septum is a muscular wall that separates the upper chambers of the heart called atria. An ASD is a common congenital heart disease where the septum is not formed properly producing a left-to-right shunt, which leads to mixing of oxygenated and deoxygenated blood. This causes pulmonary hypertension and right heart enlargement.

What are the treatment options for ASD?
Small atrial defects do not need any treatment and close on its own. Even in adulthood small ASDs may remain asymptomatic. Some large defects that persists in adulthood may become symptomatic and need closure. The ASDs can be closed by:
- Percutaneous closure using a device
- Closure through open heart surgery
Percutaneous device closure is the preferred treatment for certain defects type.
What is Percutaneous Closure of Atrial Septal Defect (ASD)?
A noninvasive procedure known as percutaneous transcatheter approach is considered depending on the size and severity of the defect. Moderate to large-sized ASD along with pulmonary hypertension requires to be closed. The procedure is performed by inserting a special closure device either folded or attached to a catheter into the vein of the leg and is advanced to the heart through the defect, which closes the hole by a special mechanism.
Are there risks associated with the procedure?
The success rate of the procedure is about 95%. But the risks involved, and their estimated incidence of occurrence include:
- Device dislodgement leading to emergency heart surgery: 1%
- Device erosion (device eroding through the heart walls): 0.3%
- Death: less than 1% usually due to perforation of the heart chamber
- Dislodgement of clot or air bubbles to the brain leading to other organs: less than 1%
- Arrhythmia: 1 to 2%
- Allergic dye reaction
- Anaesthetic reaction
- Injury to the artery/vein/nerves in the groin
- Perforation of the oesophagus
- Infection
- Allergic reaction to the nickel component of the device
Patients with small ASD may not develop any complications, but large-sized defects may lead to serious complications which demands surgery and prolonged hospitalization.
What is the pre-procedure work-up?
- Chest x-ray
- Electrocardiogram
- Blood tests
- Kidney function
A detailed diagnosis of the defect should be performed which includes transthoracic and transoesophageal echocardiogram used to assess the size, location and the suitability of the procedure.
How should I prepare for the procedure?
- Patients wearing dentures, glasses or a hearing assist device can plan to wear them during the procedure.
- Patient will be instructed about dietary restriction to be followed before the procedure.
Are there any specific instructions about medications?
- The healthcare provider may ask you to stop certain medications, such as warfarin or other blood thinners.
- If diabetic, consult the physician about how the medication needs to be adjusted.
- Provide information about specific allergies regarding iodine, shellfish, X-ray dye, latex or rubber products etc.
What happens during the procedure?
- The patient might be asked to have a shower before the procedure.
- The patient is asked to wear a hospital gown and lie on an X-ray table where an X-ray camera will move over the chest during the procedure.
- Arrangements for intravenous administration of medications or fluids during the procedure will be made.
- The site where the catheter will be inserted is cleaned and sterile drapes were used to cover the site to prevent the infection.
- Electrodes will be placed on the chest and are attached to an electrocardiograph monitor (ECG).
- A sedative might be given to relax, and a local anesthetic is given to numb the site of catheter introduction.
- A plastic sheath will be inserted in the groin, through which a catheter is inserted and threaded to the heart.
- The physician may also inject a dye which may make you feel hot or flushed for several seconds. Inform the doctor if there is an allergic reaction like itching or tightness in throat, nausea and chest discomfort.
- The X-ray cameras are used to obtain the measurements of pressures and oxygen content in the chambers.
- The appropriate size and the location of the closure might be visualized using a small catheter connected with an ultrasound transducer.
- A special catheter is used to advance the device into the heart and through the defect.
- The device is slowly pushed out of the catheter allowing each side of the device to open and close each side of the hole in the septum.
- The proper position of the device is ensured and is released from the catheter.
- It may take 1-2 hours for the procedure, but preparations must be made to spend about 5-9 hours in the hospital.
- The patient should be accompanied by someone who can drive him home, as the patient will not be allowed to drive on the same day.
What care should be taken after the procedure?
- The catheter and the imaging probe are removed after the completion of the procedure.
- Pressure on the incision site or occasionally a small suture is used to close the vein.
- Bed rest is advised for several hours to prevent bleeding, but call the doctor if you notice any bleeding.
- You might be advised to drink plenty of water to wash out the contrast material from the body.
- Your heart rate and rhythm are monitored; you may be asked to stay overnight in the hospital.
- Medications, such as aspirin are prescribed to prevent blood clots.
- Strenuous activity and heavy lifting should be avoided for at least six months.
- Antibiotic prophylaxis is required for at least six months or lifelong to prevent endocarditis, as per doctor’s advice.
- Conditions
- Acute limb ischemia
- Chronic limb ischemia
- Aortic stenosis
- Mitral valve stenosis
- Mitral valve regurgitation
- Atrial fibrillation
- Tachycardia
- Bradycardia
- Palpitations
- High blood pressure
- Atrial septal defect
- Ventricular septal defect
- Patent ductus arteriosus
- Cardiac amyloidosis
- Hypertrophic cardiomyopathy
- Varicose veins
- Deep vein thrombosis (DVT)
- Myocarditis
- Endocarditis
- Pericarditis
- Peripheral arterial disease
- Pulmonary artery hypertension
- Pulmonary embolism
- Cath lab procedures:
- Coronary Angiogram
- Primary Angioplasty
- Coronary Angioplasty
- CHIP Angioplasty
- Aortic valve replacement surgery
- Mitral valve replacement surgery
- Device closure for Atrial septal defect
- Device closure for Ventricular septal defect
- Device closure for Patent Ductus Arteriosus
- Transcatheter aortic valve replacement (TAVR)
- Inferior vena cava (IVC) filter
- LA appendage closure
- Fistuloplasty
- Balloon mitral valvotomy
- 24 hours emergency services
- Clinics- weekly basis/monthly basis/ Yearly basis
- Prevention of cardiovascular diseases
- Diagnosis
BOOK AN APPOINTMENT

Dr. RAGHU
Cardiology Coronary, Vascular and
Structural Interventions
Conditions & Diseases

Angioplasty

Aortic Stenosis

Atrial Fibrillation