Heart failure is a chronic and progressive condition that occurs when the heart cannot pump blood efficiently to meet the body’s demands. As one of the leading causes of hospitalization worldwide, managing heart failure is crucial for improving patient outcomes and quality of life. One essential aspect of heart failure management is pacing, a therapeutic approach that involves the use of electronic devices to regulate the heart’s rhythm.
In this article, we will explore the significance of pacing in heart failure, the types of pacing devices available, and their role in enhancing patient well-being.
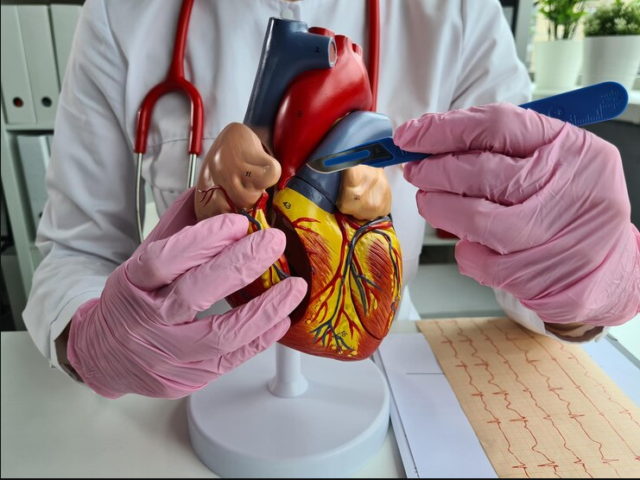
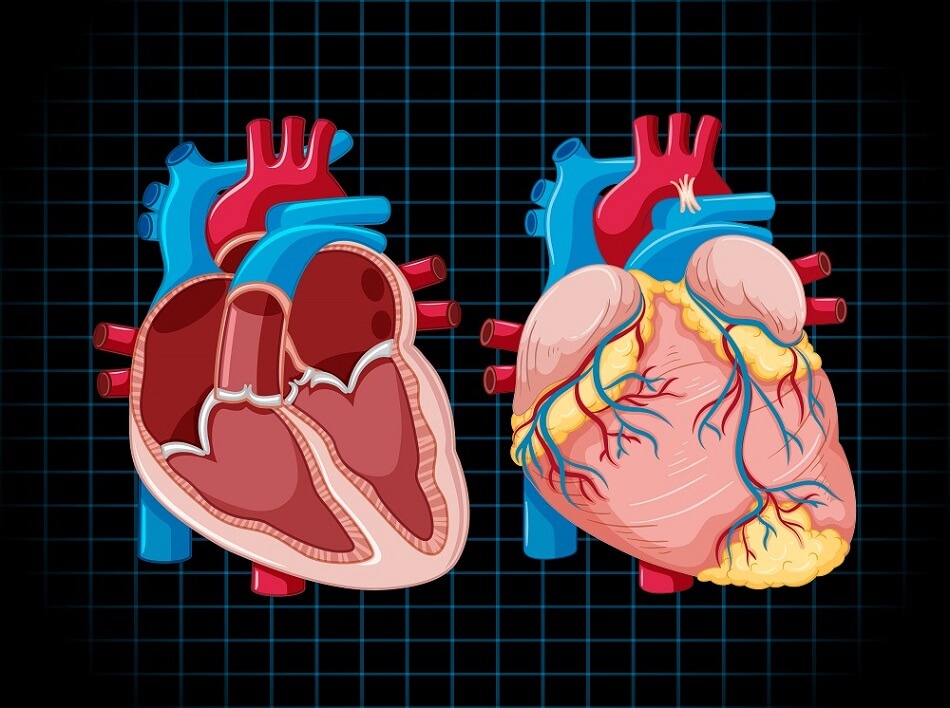
Understanding Heart Failure
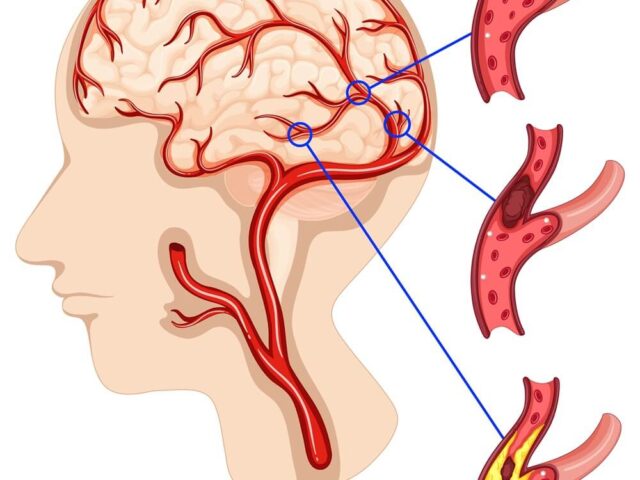
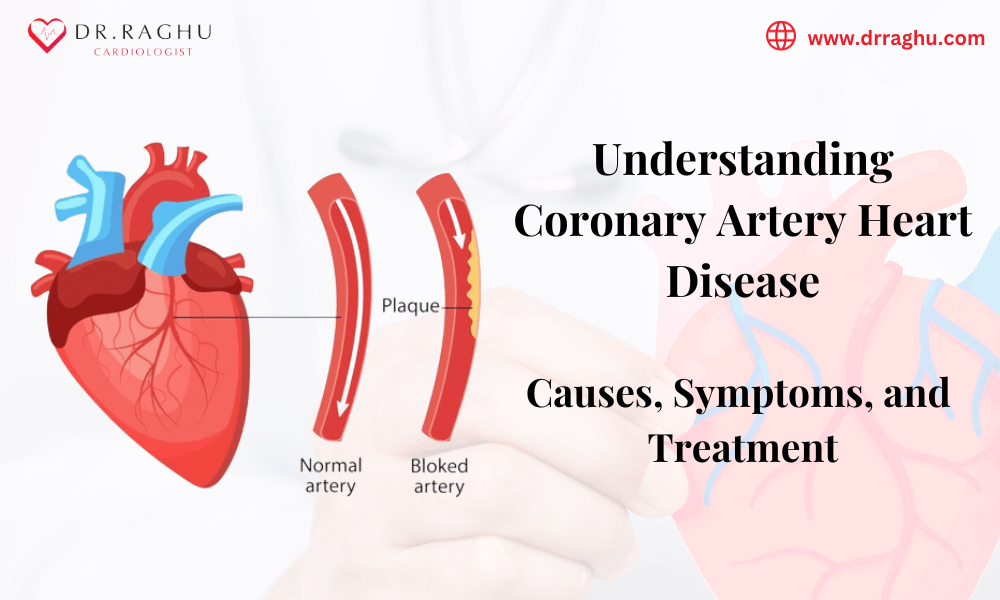
Before delving into the intricacies of pacing, it’s essential to grasp the basics of heart failure. This condition can result from various underlying causes, such as coronary artery disease, hypertension, or cardiomyopathy. As the heart weakens, it struggles to pump blood effectively, leading to symptoms like shortness of breath, fatigue, and fluid retention. The severity of heart failure is often classified into stages, ranging from mild to advanced, with pacing becoming a viable intervention in more advanced cases.
The Role of Pacing in Heart Failure Management
Pacing is a therapeutic strategy employed to regulate the heart’s rhythm and improve its pumping efficiency. In heart failure, abnormal heart rhythms (arrhythmias) can exacerbate the condition, leading to further deterioration. Pacing devices, such as pacemakers and implantable cardioverter-defibrillators (ICDs), are designed to address these issues by ensuring the heartbeats are coordinated and synchronized.
Different types of pacing devices used in heart failure treatment include:
Pacemakers
Pacemakers are small, implantable devices that regulate the heart’s rhythm by sending electrical impulses to the heart muscles. They are commonly used in cases where the heart’s natural pacemaker (the sinoatrial node) is unable to maintain a regular rhythm. Pacemakers can be further categorized into single-chamber, dual-chamber, or biventricular pacemakers, each serving specific purposes based on the patient’s condition.
Implantable Cardioverter-Defibrillators (ICDs)
ICDs are advanced pacing devices equipped with additional capabilities. In addition to pacing functions, ICDs can detect and terminate potentially life-threatening arrhythmias by delivering electrical shocks to restore a normal heart rhythm. This is particularly crucial in heart failure patients at risk of sudden cardiac death due to ventricular arrhythmias.
Cardiac Resynchronization Therapy (CRT) Devices
CRT devices, also known as biventricular pacemakers, are specifically designed for heart failure patients with impaired ventricular function. These devices synchronize the contractions of the heart’s ventricles, improving overall cardiac performance. CRT is often recommended when heart failure symptoms persist despite optimal medical therapy.
Clinical Considerations and Patient Selection
Pacing is not a one-size-fits-all solution, and careful consideration is required when determining the appropriateness of pacing devices for heart failure patients. Factors such as the underlying cause of heart failure, the severity of symptoms, and the presence of arrhythmias play a crucial role in the decision-making process. A thorough evaluation by a cardiac electrophysiologist is essential to identify the most suitable pacing strategy for each patient.
Benefits and Outcomes of Pacing Devices
Pacing devices offer significant benefits in the management of heart failure, contributing to improved patient outcomes and a better quality of life. Firstly, these devices, such as pacemakers, help regulate the heart’s rhythm, ensuring coordinated contractions that enhance cardiac efficiency.
This is vital in heart failure, where irregular heart rhythms can worsen the condition. Secondly, pacing devices improve cardiac output by optimizing heart function, leading to increased blood flow and meeting the body’s oxygen and nutrient demands more effectively.
Moreover, the use of pacing devices has been associated with a reduction in heart failure symptoms, including fatigue, shortness of breath, and exercise intolerance. By enhancing the heart’s pumping capacity, patients often experience an alleviation of these debilitating symptoms, leading to an overall improvement in well-being.
Pacing devices, particularly implantable cardioverter-defibrillators (ICDs), also play a crucial role in preventing life-threatening arrhythmias, reducing the risk of sudden cardiac death in heart failure patients.
Additionally, the impact of pacing devices extends to a broader improvement in the quality of life for heart failure patients. These devices, through advancements in technology and tailored treatment approaches, allow for a personalized management strategy.
Conclusion
Pacing has emerged as a valuable tool in the comprehensive management of heart failure, offering tailored solutions to address rhythm abnormalities and enhance cardiac function. As technology continues to advance, ongoing research and innovation in pacing devices hold the promise of further improving outcomes for heart failure patients.
With a multidisciplinary approach involving healthcare providers, cardiac electrophysiologists, and patients, pacing remains a vital component in the arsenal against this challenging cardiovascular condition.
Dr. C Raghu is a renowned cardiologist based out of Hyderabad. He specializes in interventional cardiology and has helped countless patients live longer healthier lives. If you or anyone you know is looking for heart disease treatment, reach out to Dr. Raghu today.
Book Online Consultaion
Understanding Pacing in Heart Failure Management: A Comprehensive Guide
Subscribe the Hearty Life Blogs

DR. RAGHU | Best Cardiologist in Hyderabad
Cardiology Coronary, Vascular and
Structural Interventions
Conditions & Diseases

Angioplasty

Aortic Stenosis

Atrial Fibrillation